Thursday, October 2, 2014
Scripps Research Institute Chemists Modify Antibiotic to Vanquish Resistant Bacteria
Friday, April 20, 2018
CutisPharma Announces FDA Approval of Firvanq (vancomycin) for Treatment of Clostridium Difficile Associated Diarrhea and Staphylococcus Aureus Colitis

“We are pleased to announce the FDA approval of Firvanq,” said Neal I. Muni, MD, MSPH, Chief Executive Officer of CutisPharma. “Firvanq's approval is an important step forward to providing patients the only FDA-approved vancomycin oral liquid treatment option for Clostridium difficile associated diarrhea, a life-threatening condition that affects over a half-million patients in the United States annually.”
“As a practicing infectious disease physician treating many patients with CDAD, having an FDA-approved vancomycin oral liquid formulation that is affordable and accessible to my patients is very beneficial,” said Stuart Johnson, MD, Loyola University Medical Center. “Patient access is currently limited by the fact that only a select few pharmacies perform compounding in the outpatient setting these days, given the many new regulations in place. Availability of an FDA-approved vancomycin oral liquid treatment will effectively allow any pharmacy to stock this therapy, and hopefully encourage third-party payer reimbursement, significantly improving accessibility and convenience for patients.”
Wednesday, February 7, 2018
CutisPharma Announces FDA Approval of Firvanq (vancomycin) for Treatment of Clostridium Difficile Associated Diarrhea and Staphylococcus Aureus Colitis

“We are pleased to announce the FDA approval of Firvanq,” said Neal I. Muni, MD, MSPH, Chief Executive Officer of CutisPharma. “Firvanq's approval is an important step forward to providing patients the only FDA-approved vancomycin oral liquid treatment option for Clostridium difficile associated diarrhea, a life-threatening condition that affects over a half-million patients in the United States annually.”
“As a practicing infectious disease physician treating many patients with CDAD, having an FDA-approved vancomycin oral liquid formulation that is affordable and accessible to my patients is very beneficial,” said Stuart Johnson, MD, Loyola University Medical Center. “Patient access is currently limited by the fact that only a select few pharmacies perform compounding in the outpatient setting these days, given the many new regulations in place. Availability of an FDA-approved vancomycin oral liquid treatment will effectively allow any pharmacy to stock this therapy, and hopefully encourage third-party payer reimbursement, significantly improving accessibility and convenience for patients.”
Friday, September 9, 2011
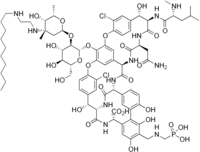
Redesigned Vancomycin As Potent Antimicrobial Activity Against Vancomycin-Resistant Bacteria...
In continuation of my update on vancomycin....
A team of scientists from The Scripps Research Institute has successfully reengineered an important antibiotic (Vancomycin) to kill the deadliest antibiotic-resistant bacteria. The researchers claim that compound could one day be used clinically to treat patients with life-threatening and highly resistant bacterial infections. The compound synthesized is an analogue of the well-known commercial antibiotic vancomycin.
Thursday, October 4, 2012
Less commonly prescribed antibiotic may be better for bloodstream infections
- 56% of patients remained on vancomycin after blood culture results reported S. aureus bacteria were susceptible to cefazolin, while only 17% were treated with cefazolin.
- Cefazolin-treated patients experienced a 38% lower rate of hospitalization and death compared with vancomycin-treated patients.
- Cefazolin-treated patients also had a 48% lower rate of sepsis, which is the most serious form of bloodstream infection.
- "I think the data suggest there is an opportunity to improve outcomes for patients through appropriate antibiotic selection," said Dr. Chan.
Monday, May 31, 2010
Plectasin - a new weapon against highly resistant microbes ?..
In this process, plectasin behaves like a thief which steals the stones off a mason. 'It binds to a cell-wall building block called lipid II and thus prevents it from being incorporated ,' Professor Sahl explains. 'However, bacteria cannot live without a cell wall.' It comes as no surprise that the most famous antibiotic penicillin also inhibits cell-wall synthesis...
Thursday, December 1, 2016
Theravance Biopharma Announces FDA Approval of Expanded Label for Vibativ (telavancin)
Expanded Vibativ Label Data
- In the all-treated cSSSI patient population with baseline S. aureus bacteremia in the ATLAS I and II trials, clinical cure rates at test-of-cure were 57.1% for Vibativ-treated patients vs. 54.6% for vancomycin-treated patients.
- In the HABP/VABP patient population with at least one Gram-positive respiratory pathogen at baseline who had concurrent S. aureus bacteremia in the ATTAIN I and II trials, the 28-day all-cause mortality rate was 40.0% for Vibativ-treated patients vs. 39.5% for vancomycin-treated patients.
Wednesday, May 25, 2011
Linezolid more effective than vancomycin in treating ventilated patients with MRSA pneumonia: Study
Linezolid more effective than vancomycin in treating ventilated patients with MRSA pneumonia: Study
Tuesday, May 12, 2015
Treatment reduces risk of recurrence of C. difficile infection
Wednesday, January 2, 2013
Sunday, June 1, 2014
FDA Approves Dalvance (dalbavancin) to Treat Skin Infections
Thursday, April 8, 2021
FDA Approves Kimyrsa (oritavancin) for the Treatment of Adult Patients with Acute Bacterial Skin and Skin Structure Infections (ABSSSI)
Melinta Therapeutics, LLC (Melinta), a commercial-stage company focused on the development and commercialization of novel antibiotics, today announced that the U.S. Food and Drug Administration (FDA) has approved Kimyrsa (oritavancin) for the treatment of adult patients with acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible isolates of designated Gram-positive microorganisms, including methicillin-resistant Staphylococcus aureus (MRSA). Kimyrsa is a lipoglycopeptide antibiotic that delivers a complete course of therapy for ABSSSI in a single, one hour 1,200 mg infusion.
“The approval of Kimyrsa demonstrates Melinta’s commitment to provide innovative therapies to patients with acute and life-threatening illnesses,” said Christine Ann Miller, President and Chief Executive Officer of Melinta. “We have responded to the requests of the medical community to provide an oritavancin product with a shorter infusion time. We believe that with the approval of Kimyrsa and product availability this summer, physicians and patients will now have a compelling new one-dose alternative to the current standard of multi-dose regimens for ABSSSI.”
ABSSSI affect approximately 14 million patients in the U.S. each year, are responsible for over 3 million visits to the Emergency Room annually and represent the 8th most common cause of Emergency Department hospital admissions1,2. ABSSSI cost U.S. hospitals $4 billion each year, with a 4.1-day average length of stay for hospitalized ABSSSI patients.2
“Kimyrsa is an important new treatment option that will provide clinicians with additional flexibility to treat ABSSSI patients in multiple care settings, without the need for hospitalization,” said Andrew Dold, D.O., member of a private infectious disease practice covering the Greater Atlanta Region. “Single-dose, long-acting antibiotics, such as Kimyrsa, may be especially beneficial for patients who lack the support or resources to adhere to multiple intravenous administrations.”
The efficacy and safety of Kimyrsa were established in the SOLO clinical trials with another oritavancin product, Orbactiv. The SOLO trials were randomized, double-blind, multicenter studies that evaluated a single 1,200 mg IV dose of oritavancin against twice-daily vancomycin for the treatment of ABSSSI in 1,987 adult patients and assessed one of the largest subsets of documented MRSA infection (405 patients). These trials demonstrated that 1,200 mg one-dose IV oritavancin infusion was as effective as 7-to-10 days of twice-daily vancomycin (1 g or 15 mg/kg) for the primary and secondary endpoints. Kimyrsa approval is based on the results of an open-label, multi-center, pharmacokinetics study, which compared Kimyrsa administered over 1 hour (N=50) to Orbactiv administered over 3 hours (N=52) for the treatment of adult patients with ABSSSI.
Michael Waters, M.D. and lead investigator in the PK clinical trial stated, “Kimyrsa was shown to be comparable to Orbactiv with a favorable safety profile. I’m pleased that these outcomes support the approval of Kimyrsa to provide oritavancin with a shorter infusion time and lower infusion volume. With these features, Kimyrsa can further enhance the treatment experience for the patient and efficiency of administration in clinical practice.”
Friday, December 30, 2016
Allergan Receives FDA Approval of Teflaro (ceftaroline fosamil) for Pediatric Patients
Tuesday, November 10, 2009
Results of Phase 3 study of fidaxomicin...

Ref : http://www.optimerpharma.com/news.asp?news_story=100&page_num=
Friday, October 28, 2016
Natural product darwinolide may help combat fatal MRSA infection

Wednesday, July 21, 2010
How honey kills bacteria..........
We know that, honey has antibiotic activity and has been used specially in burn injuries. Now researchers lead by Dr.Sebastian A.J. Zaat, of Department of Medical Microbiology at the Academic Medical Center in Amsterdam, have come up with an explanation for this antibiotic activity of honey. This first explanation to explain how honey kills bacteria. Specifically, the research shows that bees make a protein that they add to the honey, called defensin-1, which could one day be used to treat burns and skin infections and to develop new drugs that could combat antibiotic-resistant infections.
"We have completely elucidated the molecular basis of the antibacterial activity of a single medical-grade honey, which contributes to the applicability of honey in medicine," said Dr. Sebastian A.J. Zaat...
To make the discovery, Dr. Zaat and colleagues investigated the antibacterial activity of medical-grade honey in test tubes against a panel of antibiotic-resistant, disease-causing bacteria. They developed a method to selectively neutralize the known antibacterial factors in honey and determine their individual antibacterial contributions. Ultimately, researchers isolated the defensin-1 protein, which is part of the honey bee immune system and is added by bees to honey. All bacteria tested, including Bacillus subtilis, methicillin-resistant Staphylococcus aureus, extended-spectrum β-lactamase producing Escherichia coli, ciprofloxacin-resistant Pseudomonas aeruginosa, and vancomycin-resistant Enterococcus faecium, were killed by 10–20% (v/v) honey, whereas 40% (v/v) of a honey-equivalent sugar solution was required for similar activity.
After analysis, the scientists concluded that the vast majority of honey's antibacterial properties come from that protein. This information also sheds light on the inner workings of honey bee immune systems, which may one day help breeders create healthier and heartier honey bees.
http://www.fasebj.org/cgi/content/abstract/24/7/2576
Wednesday, June 26, 2013
FDA Approves Vibativ for Hospitalized Patients with Bacterial Pneumonia
Tuesday, December 8, 2009
Discovery Of Novel New Class of Antimicrobial Agents... ......
Chaperone’s antimicrobial program focuses on development of peptide as well as small molecule hsp70 inhibitor drugs that block the effect of this important class of molecular “chaperones” whose role is to help mediate or respond to toxic misfolded proteins within bacteria. Inhibition of this critical bacterial protein has been proven to kill bacterial pathogens. Besides antimicrobials, the inhibition of hsp70 molecular chaperone proteins present in other cell-types has a range of therapeutic applications that are being investigated by the company.
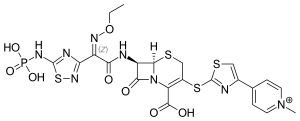
Using sophisticated computerized molecular modeling techniques, proprietary high-throughput screening tools developed by Chaperone and other approaches, the company has significantly expanded its library of novel hsp70 inhibitor compounds including CHP-267 and CHP-281, just two of the many promising drug candidates from this highly promising family of small molecule inhibitors discovered by the Company. Chaperone is looking at hsp70 inhibitors as stand alone antimicrobial agents as well as in combination with other antimicrobials (e.g., Finafloxacin.HCl : see the structure -which is under phase II clinical trials). The company recently received a US Patent covering a method of significantly amplifying the effectiveness of other antimicrobials by combining their use with that of an hsp70 inhibitor. Combining a bacterial hsp70 inhibitor with another antimicrobial yields increased bacterial killing of clinically important pathogens and the potential for combination therapy.
Source : http://www.biospace.com/news_story.aspx?NewsEntityId=118501






