An innovative treatment significantly increases the survival of people with malignant mesothelioma, a rare but rapidly fatal type of cancer with few effective treatment options, according to results from a clinical trial led by Queen Mary University of London.
The phase 3 clinical trial, led by Professor Peter Szlosarek at Queen Mary and sponsored by Polaris Pharmaceuticals, has unveiled a breakthrough in the treatment of malignant pleural mesothelioma (MPM), a rare and often rapidly fatal form of cancer with limited therapeutic options.
Mick’s journey with mesothelioma: “I have five grandchildren and two great-grandchildren now – I wouldn’t want to miss all that.”
The ATOMIC-meso trial, a randomised placebo-controlled study of 249 patients with MPM, found that a treatment – which combines a new drug, ADI-PEG20, with traditional chemotherapy – increased the median survival of participants by 1.6 months, and quadrupled the survival at 36 months, compared to placebo-chemotherapy.
The findings are significant, as MPM has one of the lowest 5-year survival rates of any solid cancer of around 5-10%. This innovative approach marks the first successful combination of chemotherapy with a drug that targets cancer's metabolism developed for this disease in 20 years.
MPM is a rare, aggressive cancer that affects the lining of the lungs and is associated with exposure to asbestos. It’s usually treated with potent chemotherapy drugs, but these are seldom able to halt the progression of the disease.
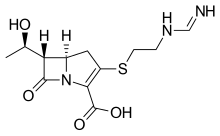
The premise behind this new drug treatment is elegant in its simplicity – starving the tumour by cutting off its food supply. All cells need nutrients to grow and multiply, including amino acids like arginine. ADI-PEG20 works by depleting arginine levels in the bloodstream. For tumour cells that can't manufacture their arginine due to a missing enzyme, this means their growth is thwarted.
The ATOMIC-meso trial is the culmination of 20 years of research at Queen Mary’s Barts Cancer Institute that began with Professor Szlosarek’s discovery that malignant mesothelioma cells lack a protein called ASS1, which enables cells to manufacture their own arginine. He and his team have since dedicated their efforts to using this knowledge to create an effective treatment for patients with MPM.
Professor Szlosarek said: “It's truly wonderful to see the research into the arginine starvation of cancer cells come to fruition. This discovery is something I have been driving from its earliest stages in the lab, with a new treatment, ADI-PEG20, now improving patient lives affected by mesothelioma. I thank all the patients and families, investigators and their teams, and Polaris Pharmaceuticals for their commitment to defining a new cancer therapy.”
Dr Tayyaba Jiwani, Science Engagement Manager at Cancer Research UK, said: "This study shows the power of discovery research which allows us to dig deep into the biology of mesothelioma to uncover vulnerabilities that we can now target with ADI-PEG20.
"Cancer Research UK is delighted to have funded the early stages of this research, including a preliminary clinical trial which established the safety and effectiveness of this drug."
There are ongoing studies assessing ADI-PEG20 in patients who have sarcoma or glioblastoma multiforme (a type of brain tumour) and other cancers dependent on arginine. The success of this novel chemotherapy in MPM also suggests that the drug may be of benefit in the treatment of multiple other types of cancer.
Mick’s journey with mesothelioma
Mick worked in a factory boiler room in the 1970s, where he was exposed to asbestos. In 2018, he visited his doctor after he began to feel unwell and had lost three stone in weight. He became anaemic and was eventually diagnosed with mesothelioma.
“It was a bit of a shock: I was given four months to live,” Mick explains. His doctor referred him to Professor Szlosarek, who enrolled him in the ATOMIC-meso trial. “I always believed in Peter. I said: ‘I’m in it to win it – you’re not getting rid of me.’ And here I am five years later.”
For two years, Mick visited St Bartholomew’s Hospital every week, accompanied by his wife, Jackie, or one of his children or grandchildren. “I’d have two injections of the new treatment – one in each arm. I didn’t have any serious side effects,” Mick explains. “I met many of the other people on the trial. Over time, some of them disappeared. But I kept going.”
Mick was awarded compensation from his former employer responsible for the asbestos exposure that ultimately led to his mesothelioma. Around 80% of mesothelioma cases are caused by workplace exposure.
Two and a half years after Mick enrolled on the ATOMIC-meso trial, his mesothelioma returned and he received a second course of treatment, this time immunotherapy. He experienced more side effects with this therapy, including encephalitis. But his cancer remains under control, and recently he was able to celebrate his 80th birthday. Professor Szlosarek and his team plan to study why certain patients, such as Mick, benefit so greatly from ADI-PEG20, in the hope of discovering how to extend this benefit to more people.
Mick says: “This trial has changed the lives of people with mesothelioma, allowing us to live longer. I have five grandchildren and two great-grandchildren now – I wouldn’t want to miss all that.”
https://jamanetwork.com/journals/jamaoncology/fullarticle/2815000


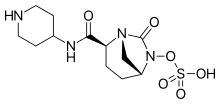 Relebactam
Relebactam