Impel NeuroPharma, Inc. (NASDAQ: IMPL), announced the U.S. Food and Drug Administration (FDA) approval of Trudhesa™ (dihydroergotamine mesylate) nasal spray (0.725 mg per spray) for the acute treatment of migraine with or without aura in adults. Trudhesa was previously known as INP104.
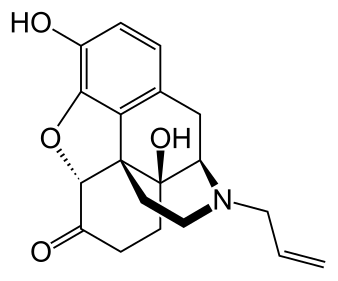
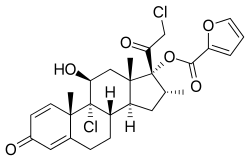
Using Impel’s proprietary Precision Olfactory Delivery (POD®) technology, Trudhesa gently delivers dihydroergotamine mesylate (DHE)—a proven, well-established therapeutic—quickly to the bloodstream through the vascular-rich upper nasal space. Trudhesa bypasses the gut and potential absorption issues, offering rapid, sustained, and consistent symptom relief without injection or infusion, even when administered hours after the onset of a migraine attack. The Commercial launch of Trudhesa is planned for early October 2021.
“We are delighted with the approval of Trudhesa and are proud to offer the millions of Americans with migraine a non-oral, acute treatment option that may provide rapid, sustained, and consistent relief, even when taken late into a migraine attack,” said Adrian Adams, Chairman and Chief Executive Officer of Impel NeuroPharma. “The approval of Trudhesa marks the culmination of more than a decade of research and advanced engineering to pair the proven efficacy of DHE with our innovative POD technology. We are grateful for all the patients and investigators who participated in our clinical trials and who were instrumental in bringing this needed advancement to the migraine community.”
The New Drug Application for Trudhesa included the results of the Phase 3, open-label, pivotal safety study, STOP 301, which is the largest longitudinal study ever conducted with DHE using nasal spray delivery. More than 5,650 migraine attacks were treated over 24 or 52 weeks during the study. The primary objective of the study was to assess the safety and tolerability of Trudhesa. Exploratory objectives included efficacy assessments of migraine measures and a patient acceptability questionnaire. In the trial, Trudhesa was generally well tolerated and exploratory efficacy findings showed it provided rapid, sustained, and consistent symptom relief. Unlike some oral acute treatments that need to be taken within one hour of attack onset to be most effective, STOP 301 reported Trudhesa offered consistent efficacy even when taken late into a migraine attack.
“Many of my patients need more from their migraine treatment, and Trudhesa offers a non-oral, fast-acting, reliable option that overcomes many current medication challenges,” said Stephanie J. Nahas-Geiger, MD, MSEd, Associate Professor in the Department of Neurology, and Program Director of the Headache Medicine Fellowship Program, Thomas Jefferson University. “Its upper nasal delivery circumvents the GI tract and common phenomena associated with migraine, such as nausea and gastroparesis, that can impact the effectiveness of oral treatments. And, importantly, it is a self-administered, single dose that can be taken anytime during a migraine attack, so patients don’t need to worry about missing the opportunity to benefit from using Trudhesa within a certain timeframe. I think patients will be very receptive to this treatment, because it pairs the long-proven benefits of DHE with a patient-friendly delivery system.”
There were no serious Trudhesa-related treatment-emergent adverse events (TEAEs) observed in the STOP 301 study and the majority of TEAEs were mild and transient in nature. Some of the most frequently reported Trudhesa-related TEAEs (≥2%) during the entire 52-week study period were nasal congestion (17.8%), nausea (6.8%), nasal discomfort (6.8%), abnormal olfactory test (6.8%) and vomiting (2.7%).
In the STOP 301 study, patient-reported exploratory efficacy findings reported that more than a third of patients (38%) had pain freedom, two-thirds (66%) had pain relief, and more than half (52%) had freedom from their most bothersome migraine symptom at two hours after their first dose of Trudhesa. For one in six patients (16%), pain relief started as early as 15 minutes. Of patients who were pain free at two hours, 93 percent were still pain free at 24 hours,11 and 86 percent were still pain free through two days. The great majority of patients (84%) reported that Trudhesa was easy to use and preferred it over their current therapy.
“Migraine is a disease that impacts the whole body and is the second leading cause of disability,” said Kevin Lenaburg, executive director, Coalition for Headache and Migraine Patients (CHAMP), which represents 12 national headache and migraine patient advocacy groups. “Historically there have not been enough effective treatments for treating migraine attacks, especially treatments that are not oral medicines, which can be challenging due to nausea, vomiting and other GI symptoms that can occur during a migraine. We welcome an important new treatment that combines the long-established efficacy of DHE with a non-oral, innovative delivery system that allows patients to self-administer wherever they are and at any point within a migraine attack.”