Ipsen (Euronext: IPN; ADR: IPSEY) announced today that the U.S. Food and Drug Administration (FDA) has approved the supplemental new drug application for Onivyde (irinotecan liposome injection) plus oxaliplatin, fluorouracil and leucovorin (NALIRIFOX) as a first-line treatment in adults living with metastatic pancreatic adenocarcinoma (mPDAC). This is the second approval for an Onivyde regimen in mPDAC, following the FDA’s approval in 2015 of Onivyde plus fluorouracil and leucovorin following disease progression with gemcitabine-based therapy.
“The results from the Phase III NAPOLI 3 trial represent the first positive data for an investigational regimen in first-line metastatic pancreatic adenocarcinoma versus the currently approved nab-paclitaxel and gemcitabine regimen,” said Christelle Huguet, EVP and Head of Research and Development, Ipsen. “With today’s approval, this Onivyde (NALIRIFOX) regimen can now offer a potential new standard-of-care treatment option with proven survival benefits for people living with metastatic pancreatic adenocarcinoma in the U.S.”
Pancreatic adenocarcinoma (PDAC) is the most common type of cancer that forms in the pancreas, with more than 60,000 people diagnosed in the U.S. each year and nearly 500,000 people globally.3,4 Since there are no specific symptoms in the early stages, PDAC is often detected late and after the disease has spread to other parts of the body (metastatic or stage IV).5 Characterized as a complex cancer due to rapid tumor progression, limited genetic targets and multiple resistance mechanisms,6 mPDAC has a poor prognosis with fewer than 20% of people surviving longer than one year.4,5 Overall, pancreatic cancer has the lowest five-year survival rate of all cancer types globally and in the U.S.4,5
“Metastatic pancreatic adenocarcinoma is a difficult disease to manage with very few available treatment options. Given the reality of this aggressive form of cancer and the complexity of the disease, every advance in the treatment landscape represents a meaningful improvement in patient outcomes.” said Dr. Zev Wainberg, Professor of Medicine and Co-Director of the UCLA GI Oncology Program. “The approval of this Onivyde regimen is an important milestone for people living with mPDAC, their families and healthcare providers, with the NAPOLI 3 trial having demonstrated survival benefits versus a current standard of care treatment option.”
“We are pleased that the U.S. Food and Drug Administration has issued this new approval of the NALIRIFOX regimen. With each new approved treatment, there is more hope for those who will be diagnosed in the future and people currently living with pancreatic cancer may have more time with their loved ones,” said Julie Fleshman, JD, MBA, President and CEO of Pancreatic Cancer Action Network (PanCAN), a patient advocacy organization committed to providing evidence-based information and resources to patients and caregivers, along with advancing research to improve patient outcomes. “We are thankful to the patients who participated in this clinical trial as they play a crucial role in advancing treatments for pancreatic cancer.”
https://en.wikipedia.org/wiki/Irinotecan



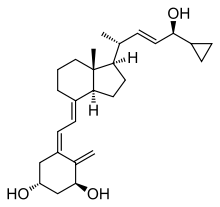 Calcipotriol
Calcipotriol

