Today, the U.S. Food and Drug Administration approved Pivya (pivmecillinam) tablets for the treatment of female adults with uncomplicated urinary tract infections (UTIs) caused by susceptible isolates of Escherichia coli, Proteus mirabilis and Staphylococcus saprophyticus.
“Uncomplicated UTIs are a very common condition impacting women and one of the most frequent reasons for antibiotic use,” said Peter Kim, M.D., M.S., director of the Division of Anti-Infectives in the FDA’s Center for Drug Evaluation and Research. “The FDA is committed to fostering new antibiotic availability when they prove to be safe and effective, and Pivya will provide an additional treatment option for uncomplicated UTIs.”
Uncomplicated UTIs are bacterial infections of the bladder in females with no structural abnormalities of their urinary tract. Approximately one-half of all women experience at least one UTI in their lifetime.
Pivya’s efficacy in treating females 18 years of age or older with uncomplicated UTIs was assessed in three controlled clinical trials comparing different Pivya dosing regimens to placebo, to another oral antibacterial drug and to ibuprofen (an anti-inflammatory drug). The primary measure of efficacy for the three trials was the composite response rate, which included clinical cure (resolution of the symptoms of the uncomplicated UTI that were present in patients at trial entry and no new symptoms) and microbiological response (demonstration that the bacteria cultured from patients’ urine at trial entry was reduced). The composite response rate was assessed approximately 8 to 14 days after patients were enrolled into the studies. In the clinical trial comparing Pivya to placebo, 62% of the 137 subjects who received Pivya achieved the composite response compared to 10% of the 134 who received placebo. In the clinical trial comparing Pivya to another oral antibacterial drug, 72% of the 127 subjects who received Pivya achieved composite response compared to 76% of the 132 who received the comparator drug. In the clinical trial comparing Pivya to ibuprofen, 66% of the 105 subjects who received Pivya achieved composite response compared to 22% of the 119 who received ibuprofen.
The most common side effects of Pivya included nausea and diarrhea.
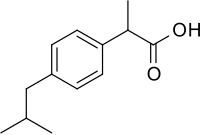
Patients should not use Pivya if they have a known history of severe hypersensitivity to Pivya or other beta-lactam antibacterial drugs. Patients should also not use Pivya if they have primary or secondary carnitine deficiency resulting from inherited disorders of mitochondrial fatty acid oxidation and carnitine metabolism, or if they are suffering from porphyria.
Pivya comes with certain warnings and precautions such as hypersensitivity reactions, severe cutaneous adverse reactions, carnitine depletion, Clostridioides difficile-associated diarrhea and interference with a newborn screening test for isovaleric acidemia, a rare metabolic disorder.
Pivya was granted Priority Review and Qualified Infectious Disease Product designations for this indication.
The FDA granted the approval of Pivya to UTILITY therapeutics Ltd.