The U.S. Food and Drug Administration approved Aurlumyn (iloprost) injection to treat severe frostbite in adults to reduce the risk of finger or toe amputation.
"This approval provides patients with the first-ever treatment option for severe frostbite,” said Norman Stockbridge, M.D., Ph.D., director of the Division of Cardiology and Nephrology in the FDA’s Center for Drug Evaluation and Research. “Having this new option provides physicians with a tool that will help prevent the lifechanging amputation of one’s frostbitten fingers or toes."
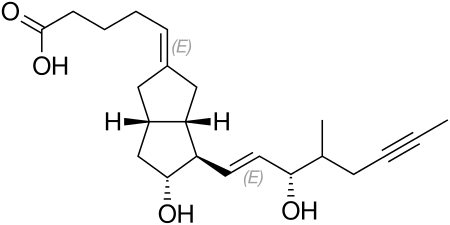
Frostbite can occur in several stages, ranging from mild frostbite that does not require medical intervention and does not cause permanent skin damage, to severe frostbite when both the skin and underlying tissue are frozen and blood flow is stopped, sometimes requiring amputation. Iloprost, the active ingredient in Aurlumyn, is a vasodilator (a drug that opens blood vessels) and prevents blood from clotting.
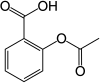
Iloprost’s efficacy in treating severe frostbite was primarily established in an open-label, controlled trial that randomized 47 adults with severe frostbite, who all received aspirin by vein and standard of care, into one of three treatment groups. One of these groups (Group 1) received iloprost by vein (intravenously) for 6 hours daily for up to 8 days. The two other groups received other medications that are unapproved for frostbite, given with iloprost (Group 2) or without iloprost (Group 3). The primary measure of efficacy was a bone scan obtained 7 days after initial frostbite that was used to predict the need for amputation of at least one finger or toe.
On day 7, the bone scan finding predictive of needing amputation was observed in 0% (0 of 16) patients receiving iloprost alone (Group 1) compared to 19% (3 of 16) patients in Group 2 and 60% (9 of 15) patients in Group 3. The presence of the bone scan abnormality was significantly lower in the two groups receiving iloprost. Most patients had follow-up information on whether they subsequently underwent at least one finger or toe amputation. The need for amputation was consistent with the bone scan findings.
The most common side effects of Aurlumyn include headache, flushing, heart palpitations, fast heart rate, nausea, vomiting, dizziness, and hypotension (blood pressure that is too low). Aurlumyn also has a warning and precaution noting that it may cause symptomatic hypotension.
Aurlumyn received Priority Review and Orphan Drug designations for this indication.
Iloprost was originally approved in 2004 for the treatment of pulmonary arterial hypertension. The FDA granted the approval of Aurlumyn to Eicos Sciences Inc.
Ref; https://en.wikipedia.org/wiki/Iloprost.