Thursday, July 21, 2022
FDA Approves Amvuttra (vutrisiran) for the Treatment of the Polyneuropathy of Hereditary Transthyretin-Mediated Amyloidosis in Adults
Thursday, June 16, 2022
FDA Approves Mounjaro (tirzepatide) Injection for the Treatment of Adults with Type 2 Diabetes
The U.S. Food and Drug Administration (FDA) has approved Mounjaro (tirzepatide) injection, Eli Lilly and Company's (NYSE: LLY) new once-weekly GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes. Mounjaro has not been studied in patients with a history of pancreatitis and is not indicated for use in patients with type 1 diabetes mellitus.
As the first and only FDA-approved GIP and GLP-1 receptor agonist, Mounjaro is a single molecule that activates the body's receptors for GIP and GLP-1, which are natural incretin hormones.1
"Mounjaro delivered superior and consistent A1C reductions against all of the comparators throughout the SURPASS program, which was designed to assess Mounjaro's efficacy and safety in a broad range of adults with type 2 diabetes who could be treated in clinical practice. The approval of Mounjaro is an exciting step forward for people living with type 2 diabetes given the results seen in these clinical trials," said Juan Pablo Frías, M.D., Medical Director, National Research Institute and Investigator in the SURPASS program.
Mounjaro will be available in six doses (2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, 15 mg) and will come in Lilly's well-established auto-injector pen with a pre-attached, hidden needle that patients do not need to handle or see.
The approval was based on results from the phase 3 SURPASS program, which included active comparators of injectable semaglutide 1 mg, insulin glargine and insulin degludec. Efficacy was evaluated for Mounjaro 5 mg, 10 mg and 15 mg used alone or in combination with commonly prescribed diabetes medications, including metformin, SGLT2 inhibitors, sulfonylureas and insulin glargine. Participants in the SURPASS program achieved average A1C reductions between 1.8% and 2.1% for Mounjaro 5 mg and between 1.7% and 2.4% for both Mounjaro 10 mg and Mounjaro 15 mg. While not indicated for weight loss, mean change in body weight was a key secondary endpoint in all SURPASS studies. Participants treated with Mounjaro lost between 12 lb. (5 mg) and 25 lb. (15 mg) on average.1
Side effects reported in at least 5% of patients treated with Mounjaro include nausea, diarrhea, decreased appetite, vomiting, constipation, indigestion (dyspepsia), and stomach (abdominal) pain. The labeling for Mounjaro contains a Boxed Warning regarding thyroid C-cell tumors. Mounjaro is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2.1
"Lilly has a nearly 100-year heritage of advancing care for people living with diabetes – never settling for current outcomes. We're not satisfied knowing that half of the more than 30 million Americans living with type 2 diabetes are not reaching their target blood glucose levels," said Mike Mason, president, Lilly Diabetes. "We are thrilled to introduce Mounjaro, which represents the first new class of type 2 diabetes medication introduced in almost a decade and embodies our mission to bring innovative new therapies to the diabetes community."
Tuesday, June 14, 2022
FDA Approves Radicava ORS (edaravone) for the Treatment of Amyotrophic Lateral Sclerosis (ALS)
"At MTPA, patients have been the driving force behind our work as we strive to develop meaningful treatment options for ALS and continue to tackle unmet needs," said Atsushi Fujimoto, President, MTPA. "Five years ago, we proudly launched Radicava as a treatment option for patients with ALS in the U.S. Now, we continue to push the boundaries of innovation with Radicava ORS, an orally administered option allowing patients flexibility in how they take their medicine."
Radicava ORS is specifically formulated for patients with ALS and provides a flexible administration option (taken orally or via feeding tube) with a small, 5 mL dose, a portable bottle, an oral dosing syringe and no need for patients to refrigerate or reconstitute before taking.1 With appropriate instruction from a healthcare provider (HCP), Radicava ORS may take only a few minutes to administer on treatment days.1 Radicava ORS should be taken in the morning after overnight fasting.1 To learn more about Radicava ORS, visit Radicava.com/update.
"ALS is a progressive disease that, due to its heterogenous nature, impacts patients at different rates with varying symptoms," said Tulio Bertorini, M.D., Professor of Neurology, The University of Tennessee Health Science Center. "Therefore, it is crucial that patients have treatment and formulation options that accommodate their own unique needs, and Radicava ORS provides HCPs who have prescribed their ALS patients edaravone with an alternate delivery option."
The comprehensive clinical development program for edaravone in ALS has spanned over a decade and included multiple clinical trials for the IV and oral formulations. The FDA approval of Radicava ORS is supported by several studies, including data from the pivotal Phase 3 clinical trial (MCI186-19) evaluating 137 ALS patients that showed treatment with Radicava slowed the loss of physical function by 33 percent (approximately one-third) compared to placebo at 24 weeks, as measured by the ALS Functional Rating Scale-Revised (ALSFRS-R), a validated rating instrument for monitoring disease progression in patients.1Additionally, seven Phase 1 clinical pharmacology studies were conducted to examine the pharmacokinetics, safety, drug-to-drug interactions, dosing, bioavailability and bioequivalence of Radicava ORS in healthy individuals and ALS patients with and without a percutaneous endoscopic gastrostomy (PEG) tube/nasogastric (NG) tube, as well as a global Phase 3, 24-week trial demonstrating the safety and tolerability profile of the treatment in 185 patients with ALS. Lastly, there is an ongoing Phase 3 study evaluating the long-term safety and tolerability of Radicava ORS for up to 96 weeks.
The most common adverse events that occurred in greater than 10 percent of patients treated with Radicava were bruising (contusion), problems walking (gait disturbance) and headache. Fatigue was observed in 7.6 percent of patients taking Radicava ORS. Radicava and Radicava ORS are contraindicated in patients with a history of hypersensitivity to edaravone or any of the inactive ingredients of this product.1 Hypersensitivity reactions and anaphylactic reactions have been reported in patients treated with Radicava.
Monday, June 13, 2022
Voquezna Triple Pak (amoxicillin, clarithromycin, and vonoprazan) FDA Approval
The Voquezna Triple and Dual Paks offer physicians the flexibility of two different treatment options. The Voquezna Triple Pak contains clarithromycin that is not included in the Voquezna Dual Pak.
Voquezna Triple Pak (amoxicillin, clarithromycin, and vonoprazan) is a co-packaged product containing amoxicillin (penicillin class antibacterial), clarithromycin (macrolide antimicrobial), and vonoprazan (potassium-competitive acid blocker (PCAB)) indicated for the treatment of Helicobacter pylori (H. pylori) infection in adults.
https://en.wikipedia.org/wiki/Amoxicillin
https://en.wikipedia.org/wiki/Clarithromycin
https://en.wikipedia.org/wiki/Vonoprazan
Saturday, June 11, 2022
FDA Approves Camzyos (mavacamten) for the Treatment of Symptomatic NYHA Class II-III Obstructive Hypertrophic Cardiomyopathy
In continuation of my update on mavacamten
Bristol Myers Squibb (NYSE: BMY) announced the U.S. Food and Drug Administration (FDA) approval of Camzyos (mavacamten, 2.5 mg, 5 mg, 10 mg, 15 mg capsules) for the treatment of adults with symptomatic New York Heart Association (NYHA) class II-III obstructive hypertrophic cardiomyopathy (obstructive HCM) to improve functional capacity and symptoms. Camzyos is the first and only FDA-approved allosteric and reversible inhibitor selective for cardiac myosin that targets the underlying pathophysiology of obstructive HCM.
“This is a first-in-class medicine specifically for patients living with symptomatic obstructive HCM,” said Milind Desai, M.D., MBA, director of the Hypertrophic Cardiomyopathy Center and director of clinical operations in Cleveland Clinic’s Heart Vascular & Thoracic Institute. "With this FDA approval, U.S. cardiologists now have a new pharmacological option for eligible patients that targets the underlying pathophysiology of the disease.”
The full U.S. Prescribing Information for Camzyos includes a Boxed WARNING for the risk of heart failure. Camzyos reduces left ventricular ejection fraction (LVEF) and can cause heart failure due to systolic dysfunction. Echocardiogram assessments of LVEF are required prior to and during treatment with Camzyos. Initiation of Camzyos in patients with LVEF <55% is not recommended. Interrupt Camzyos if LVEF is <50% at any visit or if the patient experiences heart failure symptoms or worsening clinical status. Concomitant use of Camzyos with certain cytochrome P450 inhibitors or discontinuation of certain cytochrome P450 inducers may increase the risk of heart failure due to systolic dysfunction; therefore, the use of Camzyos is contraindicated with moderate to strong CYP2C19 inhibitors or strong CYP3A4 inhibitors, and moderate to strong CYP2C19 inducers or moderate to strong CYP3A4 inducers. Because of the risk of heart failure due to systolic dysfunction, Camzyos is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the Camzyos REMS PROGRAM. Please see additional Important Safety Information including Boxed WARNING below.
“This approval builds on decades of cardiovascular leadership and reflects our steadfast commitment to people impacted by cardiovascular disease,” said Samit Hirawat, M.D., executive vice president and chief medical officer, Global Drug Development, Bristol Myers Squibb. “We are proud to bring this first-of-its kind medicine to patients, which may help to address an unmet need in the U.S. in the symptomatic NYHA class II-III obstructive HCM treatment landscape.”
This approval is based on data from the Phase 3 EXPLORER-HCM trial. At baseline, approximately 73% of the randomized patients were NYHA class II and 27% were NYHA class III. The mean LVEF was 74%, and the mean Valsalva left ventricular outflow tract (LVOT) gradient was 73 mmHg. The baseline mean Kansas City Cardiomyopathy Questionaire-23 (KCCQ-23) Clinical Summary Score (CSS) was 71. At Week 30, 37% (n=45/123) of patients taking Camzyos achieved the composite primary endpoint, defined as the proportion of patients who achieved either improvement of mixed venous oxygen tension (pVO2) by ≥1.5 mL/kg/min plus improvement in NYHA class by at least 1 or improvement of pVO2 by ≥3.0 mL/kg/min plus no worsening in NYHA class, versus 17% (n=22/128) treated with placebo. The difference was 19% (95% CI: 9, 30; p=0.0005). Additionally at Week 30, patients receiving Camzyos had greater improvement compared to placebo group across all secondary endpoints, including:
- Mean change from baseline post-exercise LVOT peak gradient [-47 mmHg vs -10 mmHG; -35 difference (95% CI: -43, -28; p<0.0001)]
- Mean change from baseline in pVO2 [1.4 mL/kg/min vs -0.1 mL/kg/min; 1.4 difference (95% CI: 0.6, 2.1; p<0.0006)]
- Number (%) of patients with improvement of NYHA class ≥ 1 [80 (65%) vs 40 (31%); difference of 34% (95% CI; 22%, 45%; p<0.0001)]
- Mean change from baseline in KCCQ-23 † CSS [14 vs 4; difference of 9 (95% CI: 5, 13); p<0.0001]
- Mean change in baseline in KCCQ-23 Total Symptom Score (TSS) (12 vs 5)
- Mean change in baseline in KCCQ-23 Physical Limitations (PL) (15 vs 4)
The KCCQ-23 CSS is derived from the Total Symptom Score (TSS) and the Physical Limitations (PL) score of the KCCQ-23. The CSS ranges from 0 to 100 with higher scores representing less severe symptoms and/or physical limitations.
Missing data were not imputed to summarize the baseline and change from baseline to Week 30 values. Difference in mean change from baseline between treatment groups was estimated using a mixed model for repeated measures.
In the EXPLORER-HCM trial, adverse reactions occurring in >5% of patients and more commonly in the Camzyos group than in the placebo group were dizziness (27% vs 18%) and syncope (6% vs 2%). Mean (SD) resting LVEF was 74% (6) at baseline in both treatment groups. Mean (SD) absolute change from baseline in LVEF was -4% (8) in the Camzyos group and 0% (7) in the placebo group over the 30-week treatment period. At Week 38, following an 8-week interruption of trial drug, mean LVEF was similar to baseline for both treatment groups. Additionally, 7 (6%) patients in the Camzyos group and 2 (2%) patients in the placebo group experienced reversible reductions in LVEF to <50% (median 48%: range 35-49%) while on treatment. In all 7 patients treated with Camzyos, LVEF recovered following interruption of Camzyos.
“The approval of Camzyos represents a significant milestone for appropriate symptomatic obstructive HCM patients and their families, who have long awaited a new treatment option for this chronic and progressive disease,” said Anjali T. Owens, MD, Medical Director of the Center for Inherited Cardiac Disease and an Assistant Professor of Medicine at the Perelman School of Medicine at the University of Pennsylvania. “As a lead U.S. investigator on the EXPLORER-HCM study, I’m grateful to the patients and their families whose participation in the trial played a key role in this approval.”
Bristol Myers Squibb offers various programs and resources to address the needs of patients and caregivers, and provide support that allows for access to therapies, including Camzyos. For additional information, call 855-Camzyos (855-226-9967) 8 am to 11 pm ET, Monday through Friday.
Friday, June 10, 2022
FDA Approves Vtama (tapinarof) Cream for the Treatment of Plaque Psoriasis in Adults
Dermavant Sciences, a biopharmaceutical company dedicated to developing and commercializing innovative therapeutics in immuno-dermatology, announced that the U.S. Food and Drug Administration (FDA) has approved Vtama (tapinarof) cream, 1%, an aryl hydrocarbon receptor agonist, indicated for the topical treatment of plaque psoriasis in adults. This approval makes Vtama cream the first and only FDA-approved steroid-free topical medication in its class.
“We are delighted with our FDA-approved label for Vtama cream, which is for adults with psoriasis, regardless of disease severity, and with an unlimited duration of use. In anticipation of today’s approval, we have a fully built commercial infrastructure in place, and I am excited to say we will have product in the channel in the first week of June. As the first and only approved drug in its class in the U.S., the FDA’s approval of Vtama cream provides an effective new non-steroidal treatment option for millions of adults living with plaque psoriasis and represents a major milestone for Dermavant and its stakeholders,” said Todd Zavodnick, Chief Executive Officer of Dermavant. “At Dermavant, we are committed to advancing novel, patient-focused innovation in immuno-dermatology. As such, we are proud to have developed a topical treatment in Vtama cream that provides not only efficacy over 52 weeks but can also be used on all body areas, including on sensitive locations, such as face, skin folds, neck, genitalia, anal crux, inflammatory areas, and axillae. In addition, an approximately four month off-treatment remittive effect (median time to first worsening), leads us to believe that Vtama cream has the potential to become the preferred topical option for this chronically underserved patient population and among the physicians who treat them.”
“Following 20-plus years of minimal innovation in the topical psoriasis treatment space1,2,3,4, I believe the approval of Vtama cream is an important step in establishing a new treatment option for adults with mild, moderate and severe plaque psoriasis ,” said Mark Lebwohl, MD, FAAD, Dean for Clinical Therapeutics and Waldman Professor and Chairman Emeritus of the Kimberly and Eric J. Waldman Department of Dermatology, Icahn School of Medicine at Mount Sinai in New York and lead author of the Phase 3 studies of Vtama cream published in The New England Journal of Medicine. “As a clinician, I’m excited to finally have a versatile, once-daily, steroid-free topical treatment that is backed by extensive clinical trial data supporting its favorable safety and efficacy profile and a demonstrated remittive effect of approximately four months in patients off therapy.”
Across PSOARING 1 and PSOARING 2, Vtama cream demonstrated highly statistically significant improvement in Physician Global Assessment (PGA)6 score of “clear” (PGA=0) or “almost clear” (PGA=1) with a minimum 2-grade improvement compared with vehicle from baseline at week 12. Vtama cream also demonstrated a highly statistically significant improvement in all secondary endpoints versus vehicle, including ≥75% Improvement in Psoriasis Area and Severity Index (PASI) score (PASI-75) from baseline at week 127. The adverse event (AE) profile of Vtama cream reported in both PSOARING 1 and PSOARING 2 demonstrated that the majority of AEs were localized to the site of application and were mild to moderate in nature. The most common AEs of subjects treated with Vtama cream were folliculitis, nasopharyngitis, and contact dermatitis.
Thursday, June 2, 2022
FDA Approves Tlando (testosterone undecanoate) for Male Hypogonadism
Antares Pharma, Inc., (NASDAQ: ATRS) (the “Company”), a specialty pharmaceutical company, today announced that the U.S. Food and Drug Administration granted final approval for TLANDO™ (testosterone undecanoate), an oral treatment for testosterone replacement therapy (“TRT”) indicated for conditions associated with a deficiency or absence of endogenous testosterone, or hypogonadism in adult males.
Robert F. Apple, President and Chief Executive Officer of Antares Pharma, commented, “The FDA approval of TLANDO brings to market an oral formulation of testosterone that we believe will prove beneficial to physicians and their patients. We have recently expanded our commercial organization to 108 sales representatives and expect to leverage our relationships with urologists and endocrinologists to drive adoption of TLANDO. This approval also reinforces the opportunity for Antares to continue to drive share gains in the TRT market with both TLANDO and XYOSTED and support our future growth with an expanded commercial portfolio. We look forward to launching TLANDO commercially, which will provide a complementary treatment option to patients and clinicians in the second quarter of this year.”
“We are excited with the opportunity to commercialize TLANDO and reinforce our commitment to the TRT market. Our existing commercial capabilities and presence in the market with XYOSTED provide an important foundation for the potential commercial success of TLANDO. With an expanded commercial footprint, we expect to continue to foster our strong physician relationships to support their patient-centric care and preference for different treatment options. We believe TLANDO’s oral formulation and convenient dosing, which requires no titration, differentiates it from other treatment options. As we prepare for the commercial launch, we look forward to our sales representatives detailing a differentiated portfolio of products consisting of XYOSTED, TLANDO and NOCDURNA that will continue to deliver solutions for improved patient care,” added Joe Renda, Senior Vice President, Commercial of Antares Pharma.
Thursday, May 5, 2022
FDA Approves Xelstrym (dextroamphetamine) Transdermal System for the Treatment of Attention-Deficit/Hyperactivity Disorder (ADHD)
Noven Pharmaceuticals, Inc., awholly-ownedsubsidiary of Hisamitsu Pharmaceutical Co., Inc., today announced that the U.S. Food and Drug Administration (FDA) has approved Xelstrym (dextroamphetamine) transdermal system, CII, for the treatment of Attention-Deficit/Hyperactivity Disorder (ADHD) for adults and pediatric patients 6 years and older.1 Xelstrym is the first-and-only FDA-approved transdermal amphetamine patch.
The efficacy and safety of Xelstrym for the treatment of ADHD in pediatric patients 6 to 17 years was evaluated in a multi-center, randomized, double-blind,placebo-controlled,cross-over design, modified analog classroom study. The primary efficacy endpoint was observed as measured by the Swanson, Kotkin, Agler, M-Flynn, and Pelham Scale (SKAMP) total score demonstrating a significant separation from placebo with the use of Xelstrym. The most common adverse reactions (incidence ≥2% and greater than the rate for placebo) in pediatric patients 6 to 17 years treated with Xelstrym were decreased appetite, headache, insomnia, tic, abdominal pain, vomiting, nausea, irritability, blood pressure increased, and heart rate increased. The efficacy and safety of Xelstrym in adults was based on the comparable Xelstrym pharmacokinetic profile in adults and children, and the established bridge to adequate and well- controlled studies of lisdexamfetamine.
"The availability of Xelstrym underscores the need for a non-oral amphetamine treatment for ADHD," said Greg Mattingly, MD, Associate Clinical Professor of Psychiatry at The Washington University School of Medicine in St. Louis, Missouri. "As a once-daily transdermal patch, Xelstrym provides clinicians and their patients, many with varying daily schedules, the ability to share in the decision making process of determining when to apply and subsequently, when to remove the patch to optimize the desired benefit of individualized treatment."
Xelstrym should be applied 2 hours before an effect is needed and removed within 9 hours after application. Dose titration and final dosage should be individualized depending on clinical response and tolerability. Xelstrym will be available in dosage strengths of 4.5 mg/9 hours, 9 mg/9 hours, 13.5 mg/9 hours and 18 mg/9 hours.1
"FDA's approval of Xelstrym provides people living with ADHD a new option to manage a medication schedule that fits their individual lifestyle," said Joel Lippman, M.D., Chief Operating Officer and Chief Medical Officer, Noven Pharmaceuticals, Inc. "As the first amphetamine transdermal patch available for the treatment of ADHD in adults and pediatrics, this is a significant milestone for Noven and our goal of offering new options for clinicians, caregivers and patients for the treatment of ADHD. This approval enables our team to finalize preparations for commercial launch in the U.S. as early as the second half of this year."
Wednesday, May 4, 2022
FDA Approves Ztalmy (ganaxolone) for Seizures Associated with CDKL5 Deficiency Disorder
Marinus Pharmaceuticals, Inc. (Nasdaq: MRNS), a pharmaceutical company dedicated to the development of innovative therapeutics to treat seizure disorders, today announced that the U.S. Food and Drug Administration (FDA) has approved Ztalmy® (ganaxolone) oral suspension for the treatment of seizures associated with cyclin-dependent kinase-like 5 deficiency disorder (CDD), a rare form of genetic epilepsy, in patients two years of age and older.1 Ztalmy, the first FDA approved treatment specifically in CDD, is a neuroactive steroid that acts as a positive allosteric modulator of the GABAA receptor. It is expected to be available through a designated specialty pharmacy in July 2022.
“Today is a historic milestone not only for Marinus but for CDD patients, families and caregivers who have long been navigating the unpredictable, often devastating reality of living with uncontrolled seizures,” said Scott Braunstein, M.D., Chief Executive Officer of Marinus. “The approval of Ztalmy would not have been possible without the patients, caregivers and investigators who participated in the clinical trials to develop this important new therapy. We are grateful and humbled by the opportunity to bring the first and only FDA-approved treatment for seizures associated with CDD to this community.
CDD is a serious and rare genetic disorder characterized by early‑onset, difficult‑to‑control seizures and severe neuro‑developmental impairment.2 It’s caused by a mutation of the cyclin-dependent kinase-like 5 (CDKL5) gene, located on the X chromosome. The CDKL5 gene produces a protein that is important for normal brain development and function. 3
“There has been a great unmet medical need for treatments that address seizures associated with CDKL5 deficiency disorder given their prominent role and profound impact on patients,” said Scott Demarest, M.D., Principal Investigator (PI) for the Marigold trial and neurologist and Clinical Director of Precision Medicine at Children’s Hospital Colorado. “To date, antiseizure treatment decisions have been based on very limited clinical evidence in this patient population and the resulting outcomes underscore the need for therapies that further improve seizure control. Thanks to our research and this trial, we now have the first treatment specifically approved for seizures associated with CDKL5 deficiency disorder that was shown to have a positive benefit-risk profile.” Dr. Demarest is also PI of the International CDKL5 Clinical Research Network and Assistant Professor of Pediatrics-Neurology at the University of Colorado School of Medicine.
The approval of Ztalmy in CDD is based on data from the Phase 3 Marigold double-blind placebo-controlled trial, in which 101 patients were randomized and individuals treated with Ztalmy showed a median 30.7% reduction in 28-day major motor seizure frequency, compared to a median 6.9% reduction for those receiving placebo, achieving the trial’s primary endpoint (p=0.0036). In the Marigold open label extension study, patients treated with Ztalmy for at least 12 months (n=48) experienced a median 49.6% reduction in major motor seizure frequency. In the clinical development program, Ztalmy demonstrated efficacy, safety and tolerability with the most common adverse reactions (incidence >/5% and at least twice the rate of placebo) in the Ztalmy group being somnolence, pyrexia, salivary hypersecretion and seasonal allergy.
“As the mother of a daughter living with CDD, I’ve experienced first-hand the devastating impact seizures can have on these patients,” said Karen Utley, President and Co-founder of the International Foundation for CDKL5 Research. “This approval is monumental for the CDD community—bringing not only the first approved treatment option specifically for CDD patients, but renewed hope to those who have struggled to find medications that are effective in significantly reducing the number of seizures these patients experience on a daily basis.
Ztalmy is expected to be commercially available in the U.S. in July following scheduling by the U.S. Drug Enforcement Administration. To support the CDD community, Marinus plans to launch The Ztalmy One™ Program, a comprehensive patient services program to provide assistance with product access, ongoing support to patients, caregivers and their medical teams, and financial support to eligible patients.
The FDA reviewed Ztalmy under Priority Review and granted Ztalmy orphan drug and Rare Pediatric Disease designations for the treatment of CDD. With the approval, the FDA awarded a Rare Pediatric Disease Priority Review Voucher (PRV), which Marinus plans to monetize.
Tuesday, May 3, 2022
FDA Approves Igalmi (dexmedetomidine) Sublingual Film for Acute Treatment of Agitation Associated with Schizophrenia or Bipolar I or II Disorder in Adults
BioXcel Therapeutics, Inc., a biopharmaceutical company utilizing artificial intelligence (AI) approaches to identify and develop transformative medicines in neuroscience and immuno-oncology, announced the U.S. Food and Drug Administration (FDA) approval of Igalmi™ (dexmedetomidine) sublingual film for the acute treatment of agitation associated with schizophrenia or bipolar I or II disorder in adults. Igalmi can be self-administrated by patients under the supervision of a healthcare provider. The Company is prepared to launch Igalmi in the U.S. in the second quarter of 2022.
“There are large numbers of patients who experience agitation associated with schizophrenia and bipolar disorders, and this condition has been a long-standing challenge for healthcare professionals to treat,” said Dr. John Krystal, M.D., the Robert L. McNeil, Jr. Professor of Translational Research and Chair of the Department of Psychiatry at Yale School of Medicine. “The approval of Igalmi, a self-administered film with a desirable onset of action, represents a milestone moment. It provides healthcare teams with an innovative tool to help control agitation. As clinicians, we welcome this much-needed new oral treatment option.”
An estimated 7.3 million people in the U.S. are diagnosed with schizophrenia or bipolar disorders. Up to a quarter of these people experience agitation, with episodes that can occur 10 to 17 times annually, totaling up to 25 million agitation episodes for these two patient populations per year. Agitation episodes are associated with a significant burden for patients, caregivers, and the healthcare system.
“Igalmi is the first new acute treatment for schizophrenia or bipolar disorder-associated agitation in nearly a decade and represents a differentiated approach to helping patients manage this difficult and debilitating symptom,” said Vimal Mehta, Ph.D., CEO of BioXcel Therapeutics. “With this landmark achievement of our first approved drug, we have taken a monumental step toward our mission of bringing transformative medicines in neuroscience to patients using our AI platform. We are deeply grateful to our clinical trial participants, healthcare providers, researchers, and employees for contributing to this important new therapy. We believe Igalmi has significant market-changing potential, and we are excited to execute on our commercial launch plans in the U.S. this quarter.”
The FDA approval of Igalmi is based on data from two pivotal randomized, double-blinded, placebo-controlled, parallel group Phase 3 trials evaluating Igalmi for the acute treatment of agitation associated with schizophrenia (SERENITY I) or bipolar I or II disorder (SERENITY II).
The primary endpoint was the mean change from baseline in the Positive and Negative Syndrome Scale-Excited Component (PEC) total score assessed at 2 hours following dosing. The key secondary endpoint was the earliest time where efficacy, measured by the change from baseline in PEC score, was statistically separated from placebo. PEC is an investigator-rated instrument for measuring agitation in patients that evaluates five elements associated with agitation: poor impulse control, tension, hostility, uncooperativeness, and excitement.
In both trials, Igalmi met the primary endpoint at two hours after the first dose in patients treated with the 120 mcg and 180 mcg doses, demonstrating statistically significant improvements from baseline. Igalmi also met the key secondary endpoint, demonstrating a rapid onset of action, with statistically significant separation from placebo observed at 20 minutes for both the 180 mcg and 120 mcg doses in SERENITY II and 20 minutes and 30 minutes in SERENITY I, respectively.
The most common adverse reactions (incidence ≥5% and at least twice the rate of placebo) were somnolence (drowsiness and feeling sleepy), paresthesia or oral hypoesthesia, dizziness, dry mouth, hypotension (low blood pressure) and orthostatic hypotension. All adverse drug reactions were mild to moderate in severity. While Igalmi did not exhibit any treatment-related serious adverse effects (SAEs) in Phase 3 studies, it may cause notable side effects including hypotension, orthostatic hypotension and bradycardia, QT interval prolongation, and somnolence.
Data from the pivotal Phase 3 SERENITY II trial evaluating Igalmi in bipolar disorders were published in the Journal of the American Medical Association (JAMA) on February 22, 2022.
About Agitation Associated with Schizophrenia and Bipolar Disorder
Agitation is a common and difficult-to-manage symptom associated with bipolar I or II or schizophrenia. Early identification and prompt intervention to relieve agitation are essential to avoid symptomatic escalation and the emergence of aggression. Expert consensus best-practice guidelines have recommended that agitation should be treated by a combination of behavioral calming techniques, verbal de-escalation, and medications that are voluntarily accepted by patients without coercion. The goal of using medication is to calm the patient so that he or she can be more accurately assessed by clinicians. Medication used in this manner is consistent with current guidelines, which state that the proper endpoint of medication administration is calming without inducing sleep. This approach may help avoid the costly and traumatic use of coercive techniques like physical restraint and seclusion, which may result in admission and prolonged hospitalization.
Monday, May 2, 2022
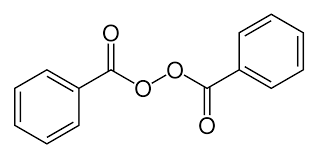
FDA Approves Epsolay (benzoyl peroxide) Cream for the Treatment of Rosacea
Sol-Gel Technologies, Ltd. a dermatology company focused on identifying, developing and commercializing branded and generic topical drug products for the treatment of skin diseases, announced today the Food and Drug Administration (FDA) approval of its drug product, Epsolay, a proprietary cream formulation of benzoyl peroxide, 5%, for the treatment of inflammatory lesions of rosacea in adults.
The benzoyl peroxide in Epsolay is encapsulated within silica-based patented microcapsules. The silica-based shell is designed to slowly release benzoyl peroxide over time to provide a favorable efficacy and safety profile. The approval of Epsolay is supported by data from two positive, identical Phase 3 randomized, double-blind, multicenter, 12-week, clinical trials that evaluated the safety and efficacy of Epsolay compared to vehicle in people with inflammatory lesions of rosacea (N = 733). The coprimary endpoints in both trials were the proportion of subjects with treatment success and the absolute change from baseline in lesion counts at Week 12. Epsolay was more effective than vehicle cream on the co-primary efficacy endpoints starting from 4 weeks of treatment in both trials. With Epsolay treatment, inflammatory lesions of rosacea were reduced by nearly 70% by the end of both 12-week trials vs. 38-46% with vehicle. Nearly 50% of subjects were ‘clear’ (IGA=0) or ‘almost clear’ (IGA=1) at 12 weeks vs. 38-46% with placebo. Post-hoc analysis of lesion count and IGA success at Week 2 confirmed a significantly greater treatment effect for Epsolay relative to vehicle as early as Week 2. In the open-label extension, 73% of subjects were ‘clear’ (IGA=0) or ‘almost clear’ (IGA=1) at 52 weeks (N = 547).
Sol-Gel has granted to Galderma Holding SA (“Galderma”) the exclusive rights to commercialize Epsolay in the United States. Founded in 1981, Galderma is the world’s largest independent dermatology company.
“Having Epsolay approved by the FDA is a watershed moment for the 16 million people in the United States suffering from rosacea,” stated Alon Seri-Levy, PhD, Chief Executive Officer of Sol-Gel. “Based on the robust clinical data, we believe that Epsolay has the potential to change the treatment landscape. We are proud to have Galderma as our partner to launch this drug since Galderma has an unparalleled track record of introducing innovative drugs in the United States’ rosacea market,” said Dr. Seri-Levy.
Neal D. Bhatia. M.D., dermatologist at Therapeutics Clinical Research in San Diego, California, commented, “There is poor adherence of my patients to current treatments for inflammatory rosacea and I look forward to being able to prescribe Epsolay to them, primarily because Epsolay has demonstrated outstanding and rapid efficacy results and also because Epsolay has been shown to be well-tolerated, both of which are important factors to ensure patients' satisfaction.”
”Galderma is committed to delivering innovation in dermatology so that healthcare professionals and their patients have the products they need,” said Baldo Scassellati Sforzolini, M.D., Ph.D., Global Head of Research & Development at Galderma. “People with rosacea experience a significant burden of disease with diminished quality of life and the approval of Epsolay represents an important advancement for those who are living with rosacea. We are pleased to be able to launch Epsolay and look forward to bringing this new treatment option to the United States.”
Monday, April 11, 2022
FDA Approves Vijoice (alpelisib) for the Treatment of PIK3CA-Related Overgrowth Spectrum (PROS)
“Today’s approval of the first treatment for PROS offers hope for a better quality of life to patients and families affected by these rare conditions,” said Kristen Davis, Executive Director of CLOVES Syndrome Community. “PROS conditions can be debilitating and disabling and can result in disruptions to everyday activities. Until today, often the only treatment options for patients were surgical or interventional radiology procedures.”
PROS conditions can affect quality of life and pose a range of physical, emotional and social challenges for patients and their families, ranging from functional impacts and developmental delays to chronic pain, mobility issues, and feelings of isolation. PROS management can be challenging, requiring collaboration from a multidisciplinary team, and patients and physicians have only had access to interventions focused on symptom management.
“I am proud of this outstanding achievement for the PROS community. The EPIK-P1 study results build on our earlier pre-clinical findings and demonstrate the efficacy of Vijoice for select PROS conditions, effectively reducing PROS growths,” said Guillaume Canaud, MD, PhD, Necker-Enfants Malades Hospital – AP-HP, the Paris Descartes University, Inserm (INEM Institute Necker Enfants Malades – Centre for Molecular Medicine). “This is a significant advancement in therapy for PROS with the potential to positively change the treatment trajectory and outcomes for patients.”
“The approval of Vijoice marks a turning point for patients who, until now, have not had an approved therapy to specifically address their disease,” said Victor Bulto, President, Novartis Innovative Medicines US. “We are grateful to the physicians, patients and families who participated in the EPIK-P1 trial. We are continuing to invest in studies to advance the scientific understanding of PROS conditions and to understand the full potential of Vijoice.”
In EPIK-P1, the most common adverse events (AEs) of any grade were diarrhea (16%), stomatitis (16%), and hyperglycemia (12%). The most common grade 3/4 AE was cellulitis (4%); one adult case was considered treatment-related
Friday, March 11, 2022
FDA Approves Leqvio (inclisiran), First-in-Class siRNA to Reduce Low-Density Lipoprotein Cholesterol (LDL-C)
"Leqvio is a revolutionary approach to lower LDL-C, and creates new possibilities for how healthcare systems can impact cardiovascular disease, a defining public health challenge of our time," said Vas Narasimhan, Novartis CEO. "We now have the opportunity, working together with partners, to provide this first-ever approved LDL-C–lowering siRNA-based therapy to tackle ASCVD at scale across the United States."
Leqvio is indicated in the United States as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with clinical atherosclerotic cardiovascular disease (ASCVD) or heterozygous familial hypercholesterolemia (HeFH) who require additional lowering of LDL-C. The effect of Leqvio on cardiovascular morbidity and mortality is being explored in clinical trials currently underway.
"ASCVD is a substantial public health burden affecting 30 million Americans," said Norman Lepor, MD, a Los Angeles based cardiologist and a clinical investigator in the Phase III clinical program for Leqvio. "As a first-of-its-kind siRNA therapy, Leqvio works differently than other cholesterol treatments, with twice-yearly dosing that makes it a compelling option for the millions of people with ASCVD already on cholesterol-lowering medications struggling to reach their LDL-C target."
Leqvio reduces the amount of LDL-C in the bloodstream by improving the liver's natural ability to prevent the production of a protein that plays a role in keeping circulating cholesterol levels high6,7. It is a subcutaneous injection given by a healthcare provider with an initial dose, then again at three months, and then every six months1. This approach may help those who have trouble sticking to medicines that are self-administered and have greater dosing frequency. Leqvio will be available in early January 2022.
"People with ASCVD have most likely experienced a heart attack or stroke from high cholesterol, causing a burden on the family and having a negative impact on lives," said Andrea Baer, Executive Director of The Mended Hearts, Inc. "One of the first steps to improving patients' health is to manage high cholesterol and we're encouraged that this new twice-a-year treatment offers a new option."
The FDA approval was based on results from the comprehensive Phase III ORION-9, -10 and -11 clinical trials, in which all 3,457 participants with ASCVD or HeFH had elevated LDL-C while receiving a maximally tolerated dose of statin therapy2,3. In the Phase III trials at month 17, Leqvio delivered effective and sustained LDL-C reduction of up to 52% vs. placebo and was reported to be well-tolerated with a safety profile shown to be comparable to placebo2,3. The most common side effects were mild to moderate injection site reaction (including pain, redness and rash), joint pain, urinary tract infection, diarrhea, chest cold, pain in legs or arms and shortness of breath2,3.
Novartis has obtained global rights to develop, manufacture and commercialize Leqvio under a license and collaboration agreement with Alnylam Pharmaceuticals, a leader in RNAi therapeutics.
Thursday, March 10, 2022
FDA Approves Recorlev (levoketoconazole) for the Treatment of Endogenous Hypercortisolemia in Adult Patients With Cushing’s Syndrome
“We are thrilled with the FDA's approval of Recorlev as a safe and effective treatment option for patients with endogenous Cushing's syndrome. With this approval, Xeris’ experienced endocrinology-focused commercial organization can begin rapidly working to help address the needs of Cushing’s syndrome patients in the U.S. who are treated with prescription therapy,” said Paul R. Edick, Chairman and CEO of Xeris Biopharma. “Today’s announcement also reinforces the value that we saw in acquiring Strongbridge Biopharma’s attractive rare disease portfolio, which we believe will deliver compelling long-term value to our shareholders. We look forward to making Recorlev commercially available in the first quarter.”
The approval of Recorlev was based upon safety and efficacy data from two positive Phase 3 studies that evaluated a combined study population of 166 patients, which was representative of the adult drug-treated U.S. population with Cushing’s syndrome. The SONICS study met its primary and key secondary endpoints, significantly reducing and normalizing mean urinary free cortisol concentrations without a dose increase. LOGICS, a double-blind, placebo-controlled randomized-withdrawal study that met its primary and key secondary endpoints, confirmed the efficacy and safety of Recorlev in normalizing and maintaining therapeutic response compared with placebo.
“Levoketoconazole (Recorlev) is an important and welcome new therapeutic option for clinicians to help manage patients with endogenous Cushing's syndrome, a severe, potentially life-threatening rare disease, if not appropriately treated, with multisystem signs and symptoms,” said Maria Fleseriu, M.D., FACE, professor of Medicine and Neurological Surgery and director of the Pituitary Center at Oregon Health Sciences University. “In prospective clinical studies, treatment with levoketoconazole was shown to be effective for reducing and normalizing cortisol.”
“Cushing’s syndrome is a rare disease that can be physically and emotionally devastating to the patient. Most patients endure years of symptoms prior to obtaining a diagnosis and are then faced with limited effective treatment options," said Leslie Edwin, president of the Cushing’s Support & Research Foundation. “Today we are excited to see that the long and complicated path of rare drug development has reached FDA approval on a new therapeutic option for our underserved Cushing's community. We are grateful that the researchers worked so diligently for so long to establish the safety and efficacy of this drug. Rare disease patients know the importance of sharing their complicated experiences as ‘expert witnesses’, and we thank Xeris for being an early adherent to this concept. We especially want to thank the clinical trial patients who made this progress possible.”
Xeris is committed to ensuring everyone who needs access to their therapies will receive it. Xeris has created Xeris CareConnection™ to provide a comprehensive program for patients and their caregivers throughout the treatment journey, including financial assistance, one-on-one support, and educational resources. Xeris CareConnection also supports healthcare professionals and their teams through education on access and reimbursement. To get started with Recorlev, reach out to Xeris CareConnection (available Monday–Friday from 8 a.m–7 p.m ET) at 1-844-444-RCLV (7258).