In continuation of my update on Sorafenib
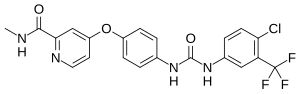
Sorafenib, a tyrosine kinase inhibitor (TKI) targeting the receptors for vascular endothelial growth factor, platelet derived growth factor, and mast/stem cell growth factor, modestly increases progression-free survival (PFS), time to progression, and disease control rate in non-small cell lung cancer (NSCLC) patients who have relapsed or failed two or three previous treatment regimens.
Lung cancer kills more people than breast, prostate, colorectal cancer combined. There are a number of treatment options now available for advanced NSCLC, the most common type of lung cancer, but almost all patients either fail or relapse after a period of clinical benefit. Patients that have relapsed or failed to respond to greater than two previous conventional chemotherapeutic treatments have very limited choices for further therapy.
A team of international investigators from 33 countries in Europe, North and South America, and Asia-Pacific conducted a relatively large phase III, randomized, double-blind, placebo-controlled trial comparing sorafenib plus best supportive care to best supportive care. This MISSION (Monotherapy admInistration of Sorafenib in patientS wIth nOn-small cell luNg cancer) trial was conducted to evaluate the efficacy and safety of sorafenib in the third or fourth-line setting with overall survival (OS) as the primary outcome measure, with PFS and other measures as a secondary endpoints.
The results published in the Journal of Thoracic Oncology, the official journal of the International Association for the Study of Lung Cancer, show that the median PFS was statistically increased in the sorafenib (N=350) vs placebo groups (N=353) (2.8 versus 1.4 months; hazard ratio [HR] 0.61; 95% confidence interval [CI] 0.51-0.72, p<0.0001), however the median OS was not different (8.2 versus 8.3 months; HR 0.99; 95% confidence interval [CI] 0.84-1.17, p=0.47). Time to progression was significantly greater (2.9 versus 1.4 months; HR 0.54; 95% CI 0.45-0.65, p<0.0001) with sorafenib than with placebo as was disease control rate (47.1% versus 24.7%, p=0.00086). Retrospective subgroup analyses showed that epidermal growth factor receptor (EGFR) mutation positive patients receiving sorafenib (N=44) had significantly longer OS (13.9 versus 6.5 months; HR 0.48; 95% CI 0.30-0.76, p=0.002) and PFS (2.7 versus 1.4 months; HR 0.27; 95% CI 0.16-0.46, p<0.001) than those receiving placebo (N=45).







