Oncology & Hematology Review, the peer-reviewed journal, has published a review highlighting recent data around rociletinib, an investigational therapy in patients with previously treated EGFR mutant-positive non-small cell lung cancer.
Treatment for patients with non-small cell lung cancer (NSCLC) is being guided increasingly by driver mutations and, routinely, tumors from patients with adenocarcinoma are screened for mutations in the kinase domain of the epidermal growth factor receptor (EGFR) as well as for other genomic abnormalities (i.e. anaplastic lymphoma kinase [ALK] and ROS1 translocations). Effective, well-tolerated treatment options that specifically target the EGFR T790M mutation (the "gatekeeper" residue) in patients with NSCLC remains an unmet need. Rociletinib is an oral, irreversible, potent, covalent inhibitor of the activating EGFR mutations (del19 and L858R) and the T790M resistance mutation; it also spares wild-type EGFR. TIGER-X is the first of the TIGER trial series, which is a clinical development program for rociletinib in patients with mutant EGFR NSCLC. This phase I-II study is evaluating rociletinib in patients who have progressed following their first and only EGFR-directed tyrosine kinase inhibitor (TKI) therapy who have developed the T790M mutation and in later-line T790M positive patients who have progressed on their second or later TKI therapy or subsequent chemotherapy. In the ongoing TIGER-X study, rociletinib has shown encouraging activity in patients with EGFR mutant-positive NSCLC and is well tolerated. Future aims of the ongoing TIGER programme include to investigate rociletinib treatment in other lines of therapy, determine whether rociletinib treatment can lead to an improvement in overall survival (OS) and to explore the potential benefits of combining rociletinib with other anti-cancer agents such as anti-programmed cell death protein and programmed cell death 1 ligand 1 monoclonal antibodies, mitogen-activated protein kinase enzyme inhibitors, vascular endothelial growth factor inhibitors, and c-Met inhibitors. Other aims include evaluating the outcome of progression-free survival associated with rociletinib treatment and determining the efficacy of rociletinib in patients with T790M negative status.



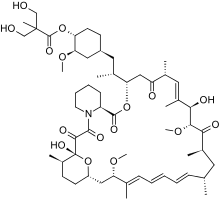 Temsirolimus
Temsirolimus Ibrutinib
Ibrutinib

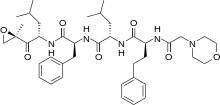
 Crizotinib
Crizotinib