The U.S. Food and Drug Administration today approved Zurampic (lesinurad) to treat high levels of uric acid in the blood (hyperuricemia) associated with gout, when used in combination with a xanthine oxidase inhibitor (XOI), a type of drug approved to reduce the production of uric acid in the body.
Gout is a painful form of arthritis caused by the buildup of too much uric acid in the body, and usually appears first as redness, soreness, and swelling in the big toe. Uric acid in the blood is produced by the breakdown of substances called purines, which are found in all the body's tissues. Uric acid usually dissolves in the blood then passes through the kidneys and out of the body in urine. Uric acid can build up in the blood, a condition called hyperuricemia. This occurs when the body increases the amount of uric acid it makes, the kidneys do not get rid of enough uric acid, or a person eats too many foods high in purines. Most people with hyperuricemia do not develop gout, but if uric acid forms crystals in the body, gout can develop.
Controlling hyperuricemia is critical to the long-term treatment of gout," said Badrul Chowdhury, M.D., director of the Division of Pulmonary, Allergy and Rheumatology Products in the FDA's Center for Drug Evaluation and Research. "Zurampic provides a new treatment option for the millions of people who may develop gout over their lifetimes."
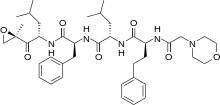
Zurampic works by helping the kidney excrete uric acid. It does this by inhibiting the function of transporter proteins involved in uric acid reabsorption in the kidney.
The safety and efficacy for Zurampic were evaluated in three randomized, placebo-controlled studies in combination with a XOI involving 1,537 participants for up to 12 months. Participants treated with Zurampic in combination with a XOI experienced reduced serum uric acid levels compared to placebo.
The most common adverse reactions in clinical trials were headache, influenza, increased blood creatinine, and gastroesophageal reflux disease.
Zurampic has a boxed warning that provides important safety information for health care professionals, including the risk for acute kidney (renal) failure, which is more common when used without an XOI and with higher than approved doses of Zurampic.
The FDA is also requiring a postmarketing study to further evaluate the renal and cardiovascular safety of Zurampic.





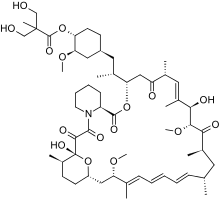 Temsirolimus
Temsirolimus Ibrutinib
Ibrutinib