An international research team has demonstrated that a new plant-derived drug can block the progression of multiple sclerosis (MS).
University of Queensland researcher Dr Christian Gruber said the breakthrough could be a step forward in preventing and treating MS and other autoimmune diseases.
"This is a really exciting discovery because it may offer a whole new quality of life for people with this debilitating disease," he said.
The new drug is expected to be taken by mouth, in contrast to some current MS treatments where patients need to have frequent injections.
MS is a chronic incurable condition marked by attacks that bring gradual deterioration in the patient's health. About 23,000 people are affected in Australia and 2.5 million worldwide.
Dr Gruber said the new drug -- named T20K -- was extracted from a traditional medicinal plant, the Oldenlandia affinis.
The drug treatment had been successful in an animal model, and patent applications filed in several countries.
"Phase one clinical trials could begin as early as 2018," Dr Gruber said.
"Licences have been assigned to Cyxone, a company established last year to develop this new class of drugs for the treatment of autoimmune diseases.
"Cyxone's immediate focus is on bringing T20K through the pre-clinical program required for delivering a safe, orally active drug."
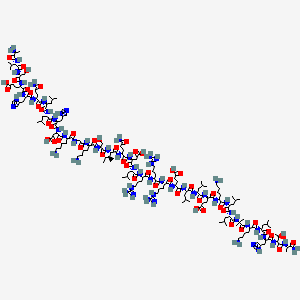
Dr Gruber said the new treatment arose from a synthesised plant peptide, a class of drugs known as cyclotides.
"Cyclotides are present in a range of common plants, and they show significant potential for the treatment of auto immune diseases," he said.
"The T20K peptides exhibit extraordinary stability and chemical features that are ideally what you want in an oral drug candidate."
New plant-derived oral drug can prevent progression of multiple sclerosis: An international research team has demonstrated that a new plant-derived drug can block the progression of multiple sclerosis (MS).