AstraZeneca today reported new Phase I extended follow-up data on osimertinib in both first- and second-line treatment of patients with non-small cell lung cancer (NSCLC), at the European Lung Cancer Conference (ELCC) 2016. Late-breaker presentations reinforced the efficacy and safety profile for osimertinib previously seen in the AURA clinical trials programme.


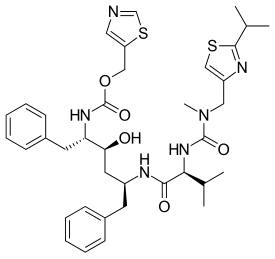
osimertinib
Phase I data from the AURA trial on osimertinib investigated as first-line treatment in 60 patients (pooled 80mg and 160mg dose cohorts) with epidermal growth factor receptor (EGFR) mutation-positive advanced NSCLC showed an objective response rate (ORR, a measurement of tumour shrinkage) of 77% (95% confidence interval (CI): 64%-87%) and a progression-free survival (PFS) of 19.3 months, with 55% of patients remaining progression-free at 18 months (95% CI: 41%-67%).1 Median duration of response (DoR) was non-calculable (NC) (95% CI: 12.5 months to NC) at the time of data cut off, with 53% of patients continuing to respond at 18 months (95% CI: 36%-67%).1 Of the 60 first-line patients, five had tumours also harbouring the T790M mutation at diagnosis (known as de novo patients) and all five of these patients showed durable responses. The most common adverse events were rash (78% overall; 2% ≥Grade 3), diarrhoea (73% overall; 3% ≥Grade 3), dry skin (58% overall; 0 ≥Grade 3) and paronychia (50% overall; 3% ≥Grade 3). All of the Grade 3 or above events in these categories occurred at the 160mg dose.
Klaus Edvardsen, Vice President, Clinical Oncology and Interim Head of Oncology, Global Medicines Development at AstraZeneca said:
In a Phase I study with osimertinib as first-line therapy in EGFR-mutation positive NSCLC, we are seeing consistently durable responses. In many cases, responses continue for at least 18 months including in a small group of patients with the T790M mutation detectable at diagnosis. The ongoing Phase III FLAURA trial will further characterise the potential of osimertinib 80mg in the first-line EGFRm setting.
AstraZeneca reports new Phase I extended follow-up data on osimertinib in NSCLC patients at ELCC 2016: AstraZeneca today reported new Phase I extended follow-up data on osimertinib in both first- and second-line treatment of patients with non-small cell lung cancer (NSCLC), at the European Lung Cancer Conference (ELCC) 2016. Late-breaker presentations reinforced the efficacy and safety profile for osimertinib previously seen in the AURA clinical trials programme.