I continuation of my update on Afitinib
Boehringer Ingelheim announced that the U.S. Food and Drug Administration (FDA) has approved a supplemental New Drug Application (sNDA) for Gilotrif® (afatinib) tablets for the treatment of patients with advanced squamous cell carcinoma of the lung whose disease has progressed after treatment with platinum-based chemotherapy. The U.S. approval follows the recent marketing authorization of Gilotrif in this patient population by the European Commission. Gilotrif, an oral, once-daily EGFR-directed therapy, is currently approved in the U.S. for the first-line treatment of specific types of EGFR mutation-positive NSCLC.
Boehringer Ingelheim announced that the U.S. Food and Drug Administration (FDA) has approved a supplemental New Drug Application (sNDA) for Gilotrif® (afatinib) tablets for the treatment of patients with advanced squamous cell carcinoma of the lung whose disease has progressed after treatment with platinum-based chemotherapy. The U.S. approval follows the recent marketing authorization of Gilotrif in this patient population by the European Commission. Gilotrif, an oral, once-daily EGFR-directed therapy, is currently approved in the U.S. for the first-line treatment of specific types of EGFR mutation-positive NSCLC.
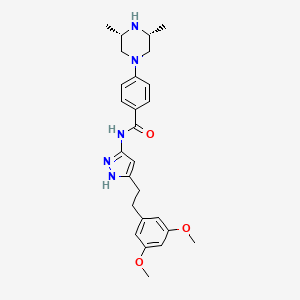
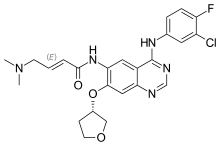 afatinib
afatinib
“We are pleased to bring a proven therapy to patients suffering from advanced squamous cell carcinoma of the lung who have progressed despite chemotherapy,” said Sabine Luik, MD, senior vice president, Medicine & Regulatory Affairs, Boehringer Ingelheim Pharmaceuticals, Inc. “This approval is further evidence of Boehringer Ingelheim’s strong commitment to bringing new treatment options to the lung cancer community.”
Squamous cell carcinoma (SqCC) of the lung is associated with a poor prognosis, limited survival and symptoms like cough and dyspnea. The median overall survival (OS) after diagnosis of advanced SqCC is around one year.
LUX-Lung 8 clinical trial investigator Shirish Gadgeel, MD, leader of the Thoracic Oncology Multidisciplinary Team at the Karmanos Cancer Center, Detroit, commented: “The overall survival data and significant delay in lung cancer progression seen in the global head-to-head Phase III trial demonstrated that Gilotrif is an effective new treatment option in this patient population.”
The sNDA was based on results of the head-to-head LUX-Lung 8 trial in patients with SqCC of the lung whose tumors progressed after first-line chemotherapy. Gilotrif, compared to erlotinib, demonstrated:
- Significant delay in progression of lung cancer (PFS, progression-free survival, primary endpoint), reducing the risk of cancer progression by 18%
- Significant improvement in overall survival (OS, key secondary endpoint), reducing the risk of death by 19%
- Significantly improved disease control rate (51% vs 40%; P=0.002)
The most common adverse reactions observed with Gilotrif (reported in at least 20% of study patients) were diarrhea (75%), rash or acne (70%), stomatitis (mouth sores) (30%), decreased appetite (25%), and nausea (21%).
LUX-Lung 8 (NCT01523587) is part of the Gilotrif LUX-Lung program – the largest collection of clinical trials of any EGFR tyrosine kinase inhibitor (TKI), with over 3,760 patients across eight studies conducted around the world. The comprehensive LUX-Lung program includes two pivotal studies in the first-line setting for EGFR mutation-positive patients, LUX-Lung 3 and LUX-Lung 6, which compared Gilotrif to chemotherapy regimens. In addition, the program included two head-to-head studies (LUX-Lung 7 and LUX-Lung 8) of Gilotrif versus first-generation EGFR TKIs gefitinib and erlotinib, respectively. The LUX-Lung program has involved over 680 sites in 40 countries, reflecting the strong partnership between Boehringer Ingelheim and the lung cancer specialist community.