In continuation of my update on Lorcaserin
Eisai Inc. and Arena Pharmaceuticals, Inc. announced the approval by U.S. Food and Drug Administration (FDA) the New Drug Application (NDA) for Belviq XR (lorcaserin HCl) CIV extended-release 20 mg tablets. The new formulation of lorcaserin will offer patients a once-a-day dosing option that may help them achieve and maintain weight loss. Belviq XR is expected to be available in the fall of 2016. In connection with the approval, Arena will receive a $10 million milestone payment.

Belviq XR is proven to be slowly absorbed in the body and lasts throughout the day. Both the original 10 mg twice-daily formulation of Belviq and newly-approved 20 mg once-daily extended release formulation are approved for use with a reduced-calorie diet and increased physical activity for chronic weight management in adults who have a body mass index (BMI) of 30 kg/m2 or greater (obese), or BMI of 27 kg/m2 or greater (overweight) with at least one weight-related medical condition, such as high blood pressure, high cholesterol, or type 2 diabetes. It is not known if Belviq or Belviq XR, when taken with other prescription, over-the-counter, or herbal weight-loss products, is safe and effective. It is not known if Belviq or Belviq XR changes your risk of heart problems, stroke, or death due to heart problems or stroke.
"With approximately two-thirds of the U.S. population living with extra weight or obesity, there is a significant and growing need to address chronic weight management," said Louis J. Aronne, M.D., Director of the Comprehensive Weight Control Center at Weill Cornell Medicine, physician at NewYork-Presbyterian/Weill Cornell Medical Center and Principal Investigator of the BELVIQ clinical trials. "Having a once-daily treatment may offer an option for patients to stay on track to meet their weight loss goals."
The bioequivalence and bioavailability of once-daily Belviq XR 20 mg compared with twice-daily Belviq 10 mg was based on two Phase 1 registrational clinical trials among healthy adult subjects. The most common treatment-emergent adverse events were similar to those seen in the Phase 3 clinical trials of Belviq 10 mg twice-daily.
"We're excited to offer this once-a-day option of lorcaserin," said Andrew Satlin, M.D., Executive Vice President, Neurology Business Group, Eisai Inc. "This option may provide another choice for patients who are overweight or obese and find it difficult to lose weight through diet and exercise alone. The development of this new formulation further underscores Eisai's ongoing commitment to help address the health care needs of this underserved population."
"We are pleased that once-daily Belviq XR has been approved by the FDA and will provide patients another option for weight loss," said Amit D. Munshi, Arena's President and Chief Executive Officer. "The approval of this new formulation is another example of Arena's success in supporting our collaborators."
What are Belviq and Belviq XR?
Belviq and Belviq XR are FDA-approved prescription weight-loss medications that, when used with diet and exercise, can help some overweight (Body Mass Index [BMI] ≥27 kg/m2) adults with a weight-related medical problem, or obese (BMI ≥30 kg/m²) adults, lose weight and keep it off.
It is not known if Belviq or Belviq XR when taken with other prescription, over-the-counter, or herbal weight-loss products is safe and effective. It is not known if Belviq or Belviq XR changes your risk of heart problems, stroke, or death due to heart problems or stroke.




 curcumin
curcumin silymarin
silymarin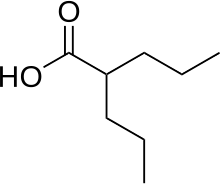 1.valproic acid
1.valproic acid