quinoxalin-2-mercapto-acetyl-urea analogs
More at : http://www.sciencedirect.com/science/article/pii/S0960894X16306643
Virus spread can be blocked by attacking Ebola's Achilles' heel.
Scientists have found Ebola's Achilles' heel: a new kind of chemical compound can block the protein Ebola uses to break out of cells and infect new cells. The compounds, revealed in a new paper in Bioorganic & Medicinal Chemistry Letters, could potentially be used to treat the disease after infection.
The outbreak of Ebola virus disease (EVD) in West Africa between 2013 and 2016 claimed more than 11,000 lives. The global public health threat has led to a resurgence in efforts to tackle the virus with scientific discovery and innovation. Many scientists are now developing vaccines, but they need to be given prophylactically and could only protect against Ebola, leaving people at risk of other hemorrhagic viruses.
Viruses replicate by hijacking the machinery in the cells of their host - in the case of Ebola, human cells - and co-opting the cells to help produce more viruses. Once production is complete, particular virus proteins promote release of viruses from the cell surface, which can go on to infect more cells.
The new compounds target an interaction between the virus and the host cell, inhibiting new Ebola viruses from escaping cells once they have been assembled. The team's results show that the compounds block this interaction without being toxic to human cells.
Dr. Harty, one of the authors of the study from the University of Pennsylvania School of Veterinary Medicine in the US, commented: "Positive results showing potent viral inhibition without toxicity to normal healthy cells may lead to a paradigm shift in the search for better antiviral drugs. Importantly, as these virus-host interactions represent a common mechanism used by a range of RNA viruses, we predict that this virus-host interaction may represent an Achilles' heel in the life cycle of RNA viruses."
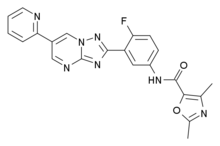
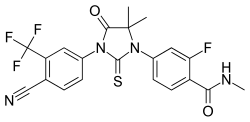
Dr. Harty and the team wanted to target the virus' mechanism for breaking out of cells, which is similar in many different RNA viruses, including Marburg and Lassa fever virus. The original virus-host interaction they modeled was between Ebola VP40 protein and host protein NEDD4. They had screened 4..8 million compounds in silico to find one that was shown to prevent VP40-NEDD4 interactions, therefore blocking virus egress.
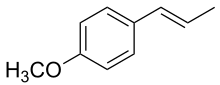
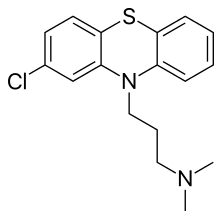
He then worked with Dr. Jay Wrobel of Fox Chase Chemical Diversity Center in the US to evaluate about 20 different commercial chemicals and this led to more potent compounds than the original hit compound. The team prepared and evaluated novel molecules that were even more potent than the original. Their efforts led to a new class of small molecule compounds that target filovirus egress. Dr. Wrobel explained:
"We postulate that emergency administration of such an antiviral therapeutics during an outbreak would inhibit virus dissemination and spread in infected individuals, thus slowing disease progression and allowing the immune system more time to mount a robust response to effectively combat and clear the infection."
The modified compounds were more than 30 times more potent than the original chemicals at inhibiting virus egress. They also showed that they do not interfere with human cell metabolism for breaking down chemicals, and are not toxic to human cells.
The research is still in the early stages. The team is now trying to get additional grants and working on even more potent chemicals with better drug-like properties so they can be tested in animal models. The next step will be for the chemicals to be tested on live viruses, then on animal models and eventually they hope to start human trials.
"This work is exciting to me since it may translate our basic science work into a potential product or therapeutic," concluded Dr. Harty.