In continuation of my update on Doxorubicin
The U.S. Food and Drug Administration today granted accelerated approval to Lartruvo (olaratumab) with doxorubicin to treat adults with certain types of soft tissue sarcoma (STS), which are cancers that develop in muscles, fat, tendons or other soft tissues. Lartruvo is approved for use with the FDA-approved chemotherapy drug doxorubicin for the treatment of patients with STS who cannot be cured with radiation or surgery and who have a type of STS for which an anthracycline (chemotherapy) is an appropriate treatment.
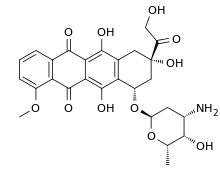
"For these patients, Lartruvo, added to doxorubicin, provides a new treatment option," said Richard Pazdur, M.D., director of the Office of Hematology and Oncology Products in the FDA's Center for Drug Evaluation and Research and acting director of the FDA's Oncology Center of Excellence. "This is the first new therapy approved by the FDA for the initial treatment of soft tissue sarcoma since doxorubicin's approval more than 40 years ago."
The National Cancer Institute estimates that 12,310 new cases of STS and nearly 5,000 deaths are likely to occur from the disease in 2016. The most common treatment for STS that cannot be removed by surgery is treatment with doxorubicin alone or with other drugs. STS includes a wide variety of tumors arising in the muscle, fat, blood vessels, nerves, tendons or the lining of the joints.
Lartruvo is a platelet-derived growth factor (PDGF) receptor-alpha blocking antibody. When stimulated, PDGF receptors cause tumor growth. Lartruvo works by blocking these receptors, which may help slow or stop tumor growth.
The safety and efficacy of Lartruvo were studied in a randomized clinical trial involving 133 patients with more than 25 different subtypes of metastatic STS. Patients received either Lartruvo with doxorubicin or doxorubicin alone. This trial measured the length of time patients lived after treatment (overall survival), the length of time tumors did not grow after treatment (progression-free survival) and the percentage of patients who experienced shrinkage of their tumors (overall response rate). Patients in this trial who received Lartruvo with doxorubicin had a statistically significant improvement in overall survival: the median survival was 26.5 months compared to 14.7 months for patients who received doxorubicin alone. Patients who received Lartruvo with doxorubicin had a median progression-free survival of 8.2 months compared to 4.4 months for patients who received doxorubicin alone. Tumor shrinkage was 18.2 percent for patients who received Lartruvo with doxorubicin and 7.5 percent for those who received doxorubicin alone.
Lartruvo has serious risks including infusion-related reactions and embryo-fetal harm. Infusion-related reactions include low blood pressure, fever, chills and rash. The most common side effects of treatment with Lartruvo are nausea, fatigue, low levels of white blood cells (neutropenia), musculoskeletal pain, inflammation of the mucous membranes (mucositis), hair loss (alopecia), vomiting, diarrhea, decreased appetite, abdominal pain, nerve damage (neuropathy) and headache.
The FDA granted the Lartruvo application fast track designation, breakthrough therapy designation and priority review status because preliminary clinical evidence indicated that it may offer a substantial improvement in effectiveness in the treatment of a serious or life-threatening disease or condition. The FDA is approving Lartruvo under the agency's accelerated approval program, which allows approval of a drug to treat a serious or life-threatening disease or condition based on clinical data showing the drug has an effect on a surrogate endpoint that is reasonably likely to predict clinical benefit. The sponsor is conducting a larger study, which is currently underway, to further explore the effectiveness of Lartruvo across the multiple subtypes of STS.
Lartruvo also received orphan drug designation, which provides incentives such as tax credits, user fee waivers and eligibility for exclusivity to assist and encourage the development of drugs intended to treat rare diseases.