Medicines Development for Global Health (MDGH) and the World Health Organisation Special Programme for Research and Training in Tropical Diseases (TDR) announced today that the United States (U.S.) Food and Drug Administration (FDA) approved moxidectin 8 mg oral for the treatment of river blindness (onchocerciasis) in patients aged 12 years and older1. The FDA has also awarded MDGH a priority review voucher (PRV).
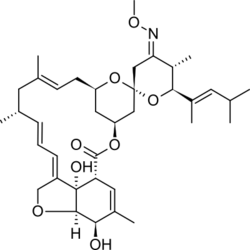
River blindness is caused by a parasitic worm, Onchocerca volvulus. The disease manifests as severe itching, disfiguring skin conditions and visual impairment, including permanent blindness, caused by the worm’s larvae (microfilariae). The approval of moxidectin was based on data from two randomized, double blind, active controlled clinical studies2,3. Each study met its respective primary endpoints, showing a statistically significant superiority of moxidectin over the current standard of care, ivermectin, in suppressing the presence of the microfilariae in skin. Full results from the Phase III study were published in the Lancet in January 20183 and a safety summary is provided below.
“FDA approval is a momentous achievement for any biopharmaceutical company, but it is a particularly rare and exciting event in the neglected diseases setting” said Mark Sullivan, Founder and Managing Director of MDGH. “It takes a broad community to develop a new medicine. FDA approval represents decades of work by thousands of scientists, disease control specialists, expert advisors, community health workers, funders and study participants. We particularly acknowledge the US$13 million investment from the Global Health Investment Fund (GHIF) as well as the extraordinary persistence and dedication of the team at TDR, without whom this would not have happened.”
TDR (the UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases) was instrumental in the development of moxidectin. “We are delighted about the FDA’s decision,” says TDR Director John Reeder. “It is a milestone toward the river blindness endgame and our objective to enable African countries to integrate moxidectin into their elimination strategies.”
This approval is the result of a paradigm-changing approach to the development of new medicines for neglected diseases, enabled by the PRV program. “As neglected tropical diseases are endemic in low and middle-income countries, there are limited markets for medicines. Therefore, finding investors willing to support development in these diseases is extremely difficult” added Mark Sullivan. “However, the introduction of the FDA’s neglected diseases PRV program has created a market around neglected diseases.“
The PRV legislation was designed to encourage development of new drug and biological products for neglected diseases. The PRV, a saleable item, permits the holder to accelerate the review of a new drug application (NDA) from the standard 10 months to 6 months. This time saving has significant value to the pharmaceutical industry, thus creating an indirect market for neglected disease treatments.
Dr. Reeder added, “This voucher to MDGH exemplifies the original spirit of the programme – to create incentives for research and development in neglected diseases.”
MDGH is the first not-for-profit company to register a medicine through the tropical disease PRV program. “This is exactly what we had in mind when we proposed the PRV program,” said Duke University’s Professor David Ridley, an author of the 2006 paper on which the voucher scheme is based. “The voucher incentive helped Medicines Development for Global Health attract funding to complete testing and registration for a drug that had been on the shelf. I’m delighted that the voucher program is playing a role in treating patients with river blindness, and one day eliminating the disease.”
“Achieving FDA approval is a critically important milestone for moxidectin, but our work to bring this medicine to those who need it most continues in earnest,” concluded Mr. Sullivan. “MDGH plans to provide the community with additional data, including data in younger children. We are here for the full journey – we have committed our skills and resources to play our part in ridding the world of this disabling disease.”
https://en.wikipedia.org/wiki/Moxidectin