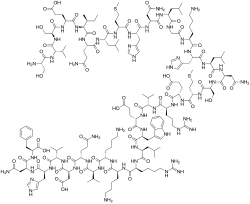
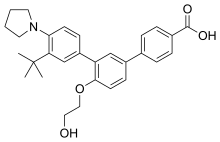
In continuation of my updates on Semaglutide
Novo Nordisk today announced that the U.S. Food and Drug Administration (FDA) has approved Rybelsus (semaglutide) tablets 7 mg or 14 mg for adults with type 2 diabetes that along with diet and exercise may improve blood sugar (glucose). Rybelsus is the first and only glucagon-like peptide-1 (GLP-1) analog in a pill and a new option for adults with type 2 diabetes who are not achieving their A1C goal with current antidiabetic treatment.
Type 2 diabetes is a global public health issue that impacts more than 28 million people in the U.S. alone.2 Despite existing treatment options, many adults with type 2 diabetes have poorly managed blood sugar that can increase the risk of developing serious diabetes-related complications.
"GLP-1 receptor agonists are effective medications for people with type 2 diabetes but have been underutilized in part because they have, until now, only been available as an injectable treatment," said Vanita R. Aroda, MD, Director of Diabetes Clinical Research, Brigham and Women's Hospital, Boston, MA and a PIONEER clinical trial investigator. "The availability of an oral GLP-1 receptor agonist represents a significant development and primary care providers, specialists and patients alike may now be more receptive to the use of a GLP-1 therapy to help them achieve their blood sugar goals."
The approval of Rybelsus is based on results from 10 PIONEER clinical trials, which enrolled 9,543 participants and included head-to-head studies of Rybelsus vs. sitagliptin, empagliflozin and liraglutide 1.8 mg.4 In the trials, Rybelsus reduced A1C and, as a secondary endpoint, showed reductions in body weight. The most common adverse reactions in the PIONEER trials, reported in ≥5% of patients, were nausea, abdominal pain, diarrhea, decreased appetite, vomiting and constipation. The types and frequency of the adverse reactions were similar across trials.
"People living with type 2 diabetes deserve more innovation, research and support to help them achieve their individual A1C goals," said Todd Hobbs, vice president and U.S. chief medical officer of Novo Nordisk. "With Rybelsus, we have the opportunity to expand use of effective GLP-1 receptor agonist therapy by providing adults with type 2 diabetes an oral medication which was previously only available as an injection to help with managing their blood sugar."
Rybelsus is approved for once-daily use in two therapeutic doses, 7 mg and 14 mg, and will be available in the U.S. beginning in Q4 2019. Initial supply of Rybelsus will come from manufacturing facilities in Denmark; however, future supply for Rybelsus will come from manufacturing facilities in the U.S. In 2015, Novo Nordisk made a strategic investment to build a new manufacturing facility in Clayton, NC to prepare for the future demand for Rybelsus. Additionally, earlier this year Novo Nordisk acquired a tableting and packaging facility in Durham, NC to meet anticipated supply needs for Rybelsus.
Novo Nordisk is working with health insurance providers with a goal of ensuring broad insurance coverage and patient access to the product. A savings card program will be available at the time of launch for eligible commercially-insured patients to keep out of pocket costs down to as little as $10 a month.
The U.S. FDA is still reviewing Novo Nordisk's new drug application (NDA) for Rybelsus seeking an additional indication to reduce the risk of major adverse cardiovascular events (MACE) such as heart attack, stroke, or cardiovascular death in adults with type 2 diabetes and established cardiovascular disease (CVD). A decision is expected in Q1 2020.
Rybelsus is currently under review by several regulatory agencies around the world, including the European Medicines Agency and the Japanese Pharmaceuticals and Medical Devices Agency.
https://en.wikipedia.org/wiki/Semaglutide