Idorsia Pharmaceuticals U.S. Inc. announced the US Food and Drug Administration (FDA) approval of Tryvio™ (aprocitentan) for the treatment of hypertension in combination with other antihypertensive drugs, to lower blood pressure in adult patients who are not adequately controlled on other drugs.1 Lowering blood pressure reduces the risk of fatal and non-fatal cardiovascular events, primarily strokes and myocardial infarctions.1 The recommended dosage of Tryvio is 12.5 mg orally once daily, with or without food.
Jean-Paul Clozel, MD and Chief Executive Officer of Idorsia commented:
"Today, there are millions of Americans whose blood pressure is not well-controlled despite existing therapies. This is a major public health issue leading to a high incidence of cardio- and cerebrovascular events. In order to help address this issue, Idorsia developed aprocitentan, an endothelin receptor antagonist suited to the treatment of these patients. Idorsia conducted an ambitious clinical program in patients remaining hypertensive despite a minimum of three drugs at their optimal dose and sometimes up to four, five, or even six antihypertensives. I'm very proud of the Idorsia team and very happy that physicians will have a new treatment option to treat patients whose blood pressure is not controlled."
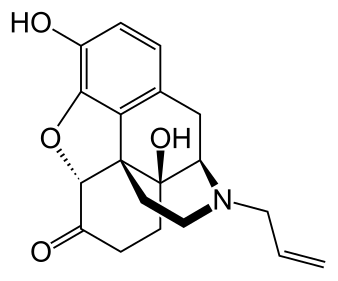
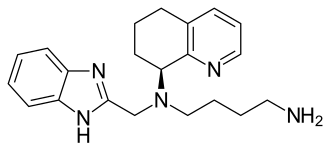
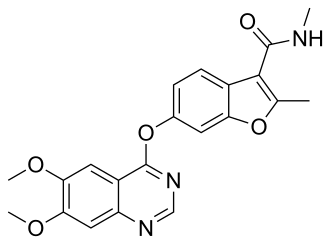
Tryvio (aprocitentan) is an endothelin receptor antagonist that inhibits the binding of endothelin (ET)-1 to ETA and ETB receptors.1,2 The effects of ET-1 bear many similarities with the pathophysiology of hypertension,3 and ET-1 is a major driver of aldosterone production.4 Until the approval of Tryvio, no systemic antihypertensive medications targeted the ET pathway,5 as approved antihypertensive therapies focus on the regulation of salt and water (diuretics), antagonism of the renin–angiotensin–aldosterone (RAAS) system, reduction of influx of extracellular calcium into the cell (calcium channel blockers), sympatholytic activity (beta blockers, central alpha-agonist agents), or non-selective vasodilatory effects.6,7
Tryvio was evaluated as a monotherapy in a Phase 2 study in patients with hypertension,8 and as an add-on therapy in a Phase 3 study called PRECISION in patients with confirmed resistant hypertension.9 In PRECISION, aprocitentan was well tolerated and superior to placebo in lowering blood pressure at week 4, with a sustained effect at week 40.10
Martine Clozel, MD and Chief Scientific Officer of Idorsia, commented:
"Early on, we realized that endothelin was involved in patients with hypertension, especially in those remaining uncontrolled despite other anti-hypertensive drugs. Since the endothelin pathway was not yet tackled in these patients, we selected aprocitentan, an endothelin receptor antagonist with the ideal properties for use in this condition. We were delighted when we saw the safety and efficacy data with Tryvio, even on top of multiple antihypertensives, in patients whose hypertension is not adequately controlled. The recognition of its potential with today's FDA approval is great news for prescribers and patients."
Michael A. Weber, MD, Professor of Medicine, Division of Cardiovascular Medicine State University of New York, and an investigator in the PRECISION study commented:
"Today, we are not able to reduce blood pressure below recommended levels in at least 10% of the hypertensive patients we treat. As well, it is often patients at high risk of adverse cardiovascular outcomes and typically with comorbidities who pose this challenge. We have had to wait for over 30 years to see the approval of an oral anti-hypertensive agent that works on a new therapeutic pathway, so Tryvio provides transformational progress in the field of systemic hypertension. It is taken as a single daily oral dose that works in combination with whatever other drugs are being prescribed and without drug-drug interactions in patients with the burden of uncontrolled hypertension. Tryvio is easy for physicians to prescribe and easy for patients to use."
Phase 3 clinical study1,9,10
The efficacy of Tryvio (aprocitentan) was evaluated in a multipart, Phase 3 multicenter study (PRECISION, NCT03541174) in adults with systolic blood pressure (SBP) ≥140 mmHg who were prescribed at least three antihypertensive medications. The trial included a placebo run-in period, which was followed by three parts as described below. Prior to the placebo run-in period, all patients were switched to standard background antihypertensive therapy consisting of an angiotensin receptor blocker, a calcium channel blocker, and a diuretic, which was continued throughout the study. Patients with concomitant use of beta‑blockers continued this treatment throughout the study.
Following the 4-week placebo run-in period, 730 patients were randomized equally to aprocitentan at either 12.5 mg, 25 mg, or placebo once daily during the initial 4-week double-blind (DB) treatment period (part 1). At the end of 4 weeks, all patients entered the single-blind treatment period (part 2) where they received 25 mg aprocitentan once daily for 32 weeks. At the end of the 32 weeks, patients were re-randomized to receive either 25 mg aprocitentan or placebo, once daily, during a 12-week DB-withdrawal period (part 3).
The primary efficacy endpoint was the change in sitting SBP (SiSBP) from baseline to Week 4 during part 1, measured at trough by unattended automated office blood pressure (uAOBP).
The key secondary endpoint was the change in SiSBP measured at trough by uAOBP from Week 36 (i.e., prior to randomized withdrawal to 25 mg aprocitentan or placebo in part 3) to Week 40.
Patients had a mean age of 62 years (range 24 to 84 years) and 60% were male. Patients were White (83%), African American (11%) or Asian (5%). Approximately 10% were Hispanic. The mean body mass index (BMI) was 34 kg/m2 (range 18 to 64 kg/m2). At baseline, 19% of patients had an eGFR 30–59 mL/min/1.73 m2 and 3% had an eGFR 15–29 mL/min/1.73 m2. At baseline, 24% of patients had a urine albumin-to-creatinine ratio (UACR) of 30–300 mg/g and 13% had a UACR >300 mg/g. Approximately 54% of patients had a medical history of diabetes mellitus, 31% ischemic heart disease, and 20% congestive heart failure. At baseline, 63% of patients reported taking four or more antihypertensive medications.
Tryvio 12.5 mg was statistically superior to placebo in reducing SiSBP at Week 4 (part 1). The treatment effect was consistent for sitting diastolic BP (SiDBP).
The persistence of the BP-lowering effect of Tryvio was demonstrated in part 3 of the trial, in which patients on aprocitentan were re-randomized to placebo or 25 mg aprocitentan following a period during which all patients were treated with 25 mg. In patients re-randomized to placebo, the mean SiSBP increased, whereas in patients re-randomized to 25 mg aprocitentan the mean effect on SiSBP was maintained and was statistically superior to placebo at Week 40. The treatment effect was consistent for SiDBP.
Most of the BP-lowering effect occurred within the first two weeks of treatment with Tryvio. Tryvio is not approved for use at a 25 mg dose. The efficacy for the 25 mg aprocitentan dose as measured in the primary end point of change in sitting SBP (SiSBP) from baseline to Week 4 in part 1, was similar to the 12.5 mg dose and thus aprocitentan 12.5 mg is the approved dose.
Tryvio's BP-lowering effect appeared consistent among subgroups defined by age, sex, race, BMI, baseline eGFR, baseline UACR, medical history of diabetes, and between BP measurement methodologies (uAOBP and ambulatory BP measurements).
The most frequently reported adverse reactions to Tryvio during the 4-week double-blind placebo-controlled treatment period (part 1) of the PRECISION study were edema/fluid retention and anemia. During the initial 4-week double-blind placebo-controlled treatment period (part 1), 0.8% of patients experienced an adverse reaction of hypersensitivity (i.e., rash, erythema, allergic edema) on Tryvio compared to no reports in patients treated with placebo. One patient experienced allergic dermatitis requiring hospitalization while receiving aprocitentan 25 mg. Tryvio is contraindicated in patients who are hypersensitive to aprocitentan or any of its excipients. Use of Tryvio is contraindicated in pregnancy.
Lowering BP reduces the risk of fatal and non-fatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes. There are no controlled trials demonstrating reduction of risk of these events with Tryvio.
Alberto Gimona, MD and Head of Global Clinical Development of Idorsia, commented:
"When designing PRECISION, we did not shy away from including patients who are most at risk of the serious negative consequences of hypertension. In addition, while all patients needed to be on three antihypertensives to join the study, 63 percent of patients were on four or more anti-hypertensives. The study was therefore truly reflective of the real-world patient population whose blood pressure is not adequately controlled on other drugs. Tryvio demonstrated a clear and consistent effect across all endpoints of blood pressure measurement and in key sub-populations. As a result, Tryvio brings hope as a novel, effective and well-tolerated treatment option for patients with hypertension not adequately controlled."
Tosh Butt, President and General Manager of Idorsia US commented:
"The approval of Tryvio in the US marks another major milestone for Idorsia. With Tryvio, we've got an innovative medicine with a unique mode of action in systemic hypertension. The team at Idorsia has a deep understanding and rich history in the field of endothelin receptor antagonism. We are eager to provide physicians and patients with a novel medicine working in a new pathway in uncontrolled hypertension that can provide additional blood pressure control. We recognize that the resources required to reach the entire prescribing community could be substantial, so we will carefully craft the Tryvio launch strategy in the coming months, while preparing to make Tryvio available during the second half of 2024."
The team at Idorsia has been working on the research and development of endothelin receptor antagonists for more than 30 years, successfully bringing three other molecules from this class to patients in different indications. ET-1, via its receptors (ETA and ETB), mediates a variety of deleterious effects such as vasoconstriction, fibrosis, cell proliferation, and inflammation. In hypertension, ET-1 can cause endothelial dysfunction, vascular hypertrophy and remodeling, sympathetic activation, and increased aldosterone synthesis.1
Martine Clozel, MD and Chief Scientific Officer of Idorsia, concluded:
"After more than 30 years working in the field of endothelin science, our research has brought about changes in the treatment paradigm of several cardiovascular diseases. Now we are bringing significant medical progress for patients with systemic hypertension. I am convinced that with the data we have seen, the approval of Tryvio heralds a new era of endothelin research beyond hypertension, where we intend to investigate the utility of aprocitentan for first-in-class applications in new indications."
Ref : https://en.wikipedia.org/wiki/Aprocitentan