Infantile spasms, a rare but severe form of epilepsy, poses significant challenges for patients and their families. Pyros is committed to providing dependable services and an affordable treatment option to help ensure that families facing an IS diagnosis, and whose children are prescribed vigabatrin can quickly obtain this essential therapy.
"The approval of Vigafyde™ marks the first new drug indicated for infantile spasms in fifteen years and underscores our unwavering commitment to supporting families facing this challenging condition," stated Michael Smith, co-founder and Chief Executive Officer of Pyros.
“This is a momentous day for patients and caregivers who have long awaited the first ready-to-use vigabatrin. I believe this approval will bring renewed energy and momentum to the infantile spasms community, enhancing our efforts to improve disease education, develop care pathways, and expand investment in infantile spasms research,” stated Edwin Urrutia, co-founder and Chief Operating Officer at Pyros.
Vigafyde™ is expected to be available in the second half of 2024. Additionally, Pyros Total Care™, the Company’s personalized comprehensive support program, is available to assist families throughout the treatment journey.
About Pyros Total Care™
As part of the Company’s commitment to prioritizing patient access to treatments for those who need them most, Pyros provides ongoing personalized support to caregivers through Pyros Total Care™ for those prescribed Vigafyde™. The support program offers personal assistance and financial resources to caregivers whose child is starting or continuing therapy.
Our dedicated support team includes a nurse educator, reimbursement support, and a clinical pharmacist. For more information, visit PyrosTotalCare.com or call 1-888-760-8330, Monday to Friday, 8 a.m. to 5 p.m. Central Time.
About Infantile Spasms
Infantile spasms (IS) is a rare, severe form of epilepsy that typically begins in children less than one year old.1 Infantile spasms can appear as subtle but repetitive movements that can often be overlooked or misdiagnosed. IS can lead to long-term permanent issues such as continued seizures, other forms of epilepsy, autism spectrum disorder, and developmental issues.2 The American Academy of Neurology conducted a systematic review of treatment for IS and concluded that successful treatment of IS can improve the long-term prognosis.3
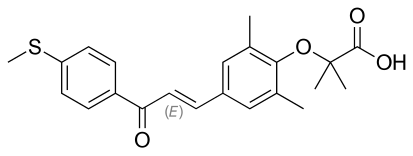
About Vigabatrin
Vigabatrin is a medication used in the treatment of infantile spasms and is designed to inhibit the enzyme GABA transaminase, consequently increasing gamma-aminobutyric acid (GABA) levels in the brain.4,5 This release is thought to enhance seizure control for patients by modulating neuronal excitability.6 Vigabatrin's mechanism of action underscores its importance in treating seizure disorders.7 Its impact may extend beyond seizure management, with emerging research indicating potential benefits in mitigating neurodevelopmental complications associated with certain epilepsy syndromes