Based on the strong evidence of effectiveness, "We should not limit or impede the use and expansion of buprenorphine therapy," write Drs. Xiaofan Li, Daryl Shorter, and Thomas Kosten, of the Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine and Michael E. DeBakey Veterans Affairs Medical Center, Houston, Texas. They propose specific strategies to promote buprenorphine use while ensuring quality of care and reducing the risk of diversion and abuse.
Focus on Expanding Buprenorphine Use 'Safely and Effectively'
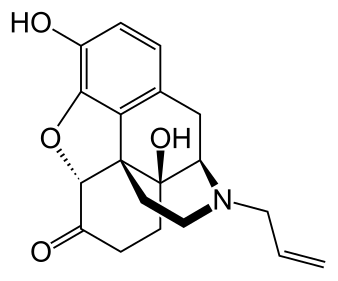
A "partial agonist" of the μ-opioid receptor in the brain, buprenorphine has similar actions to other opioids, but with less potential for abuse and a more favorable safety profile. Because it reduces demand for opioids, buprenorphine therapy is an effective deterrence strategy to combat opioid abuse. The authors cite studies suggesting that access to buprenorphine therapy can sharply reduce heroin mortality--including reductions of more than 50 percent in France and 37 percent in Baltimore.
Compared to methadone--long the standard for treating opioid and heroin addiction--buprenorphine poses lower risks related to diversion and non-medical use. The most commonly prescribed form of buprenorphine includes the opioid antagonist (blocker) naloxone, decreasing the potential for intravenous abuse.
But there are strict controls on prescribing of buprenorphine, which is classified as a Schedule III controlled substance in the United States. To prescribe buprenorphine in office-based settings, physicians must receive a Drug Enforcement Agency (DEA) waiver, complete special training, and comply with limits on the number of treated patients.
While medical use of buprenorphine has skyrocketed over the past decade, most prescribers are located in urban areas. It is estimated that 53 percent of US counties do not have any physician with a DEA waiver to prescribe buprenorphine.
Measures to make buprenorphine treatment more accessible have been proposed, such as allowing prescribing by qualified advanced nurse practitioners and physician assistants and loosening limits on number of patients treated. But these measures have been controversial, reflecting legitimate concerns about increased potential for diversion and abuse. Data show that, as use of buprenorphine to treat opioid use disorder has increased, so have the rates of misuse and diversion.
Drs. Li, Shorter, and Kosten raise special concern about the recent emergence of intravenous buprenorphine abuse. They write, "This real-world, almost paradoxical, phenomenon demonstrates the complexity inherent in the treatment of addictive disorders--a medication intended to treat substance use disorder that has its own abuse potential, upon gaining popularity and increased availability, will inevitably be explored by drug abusers for reward and reinforcement purposes."
Earlier this year, President Obama announced an initiative to increase access to effective medications for treating opioid addiction--specifically, buprenorphine and naloxone. Drs. Li, Shorter, and Kosten outline strategies to expand effective treatment with buprenorphine while reducing the risks of diversion and abuse, including:
- Additional support for physicians with high caseloads and other measures to help prescribers comply with guidelines.
- Continuing medical education targeting improvements in office-based therapy for opioid abuse.
- Policies and regulations promoting safe practice.
- Financial incentives coupled with mandatory enforcement of essential components of safe practice.
- More active pharmacy involvement, including supervised dispensing.
- Identification of groups at high risk of intravenous buprenorphine abuse.
"The question is not whether or not to expand buprenorphine prescribing," the authors add. "It is how to expand buprenorphine prescribing safely and effectively."