In continuation of my update on naloxone hydrochloride, Adamis Pharmaceuticals Corporation (Nasdaq: ADMP) announced the U.S. Food and Drug Administration (FDA) approval of Adamis’ Zimhi™ (naloxone HCL Injection, USP) 5 mg/0.5 mL product. Zimhi is a high-dose naloxone injection product FDA-approved for use in the treatment of opioid overdose.
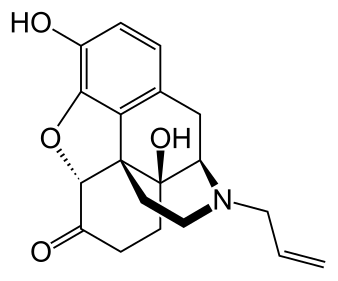
Naloxone is an opioid antagonist and is generally considered the drug of choice for immediate administration for opioid overdose. It works by blocking or reversing the effects of the opioid, including extreme drowsiness, slowed breathing, or loss of consciousness. Common opioids include morphine, heroin, tramadol, oxycodone, hydrocodone and fentanyl.
According to statistics published by the Centers for Disease Control and Prevention (CDC), drug overdoses resulted in approximately 96,779 deaths in the United States during the 12-month period ending March 2021, which was a 29% increase over the prior 12-month period. Drug overdoses are now the leading cause of death for Americans under age 50, with more powerful synthetic opioids, like fentanyl and its analogues, responsible for the largest number of those deaths.
Dr. Jeffrey Galinkin, an anesthesiologist, and former member of the FDA Advisory Committee for Anesthetics, Analgesics and Addiction Products, commented, “I am pleased to see this much needed high dose naloxone product will become part of the treatment tool kit as a countermeasure to the continued surge in fentanyl related deaths. The higher intramuscular doses of naloxone in Zimhi should result in more rapid and higher levels of naloxone in the systemic circulation, which in turn, should result in more successful resuscitations.”
Dr. Dennis J. Carlo, President and CEO of Adamis, stated, “We are very excited by this approval and are working with our commercial partner, US WorldMeds, to make this much-needed, lifesaving product readily available to the market. Zimhi provides the highest systemic levels of naloxone compared to any of the nasal or intramuscular products currently available.”
P. Breckinridge Jones, Sr., CEO of US WorldMeds, added, “We are pleased with the approval and now look forward to commercially marketing Zimhi in the United States. US WorldMeds has a proven track-record of successfully commercializing pharmaceutical products and have a First-in-Class and only FDA-approved product, LUCEMYRA® (lofexidine), for the treatment of withdrawal symptoms associated with abrupt opioid discontinuation. We are confident we can leverage our existing commercial infrastructure and presence in the opioid dependence market to speed the uptake of Zimhi and combat the growing opioid crisis. We are preparing for the full commercial launch of ZIMHI which is planned for the first quarter of 2022.”\